Case 1: Genetic testing to support disorder diagnosis
Approach/Workflow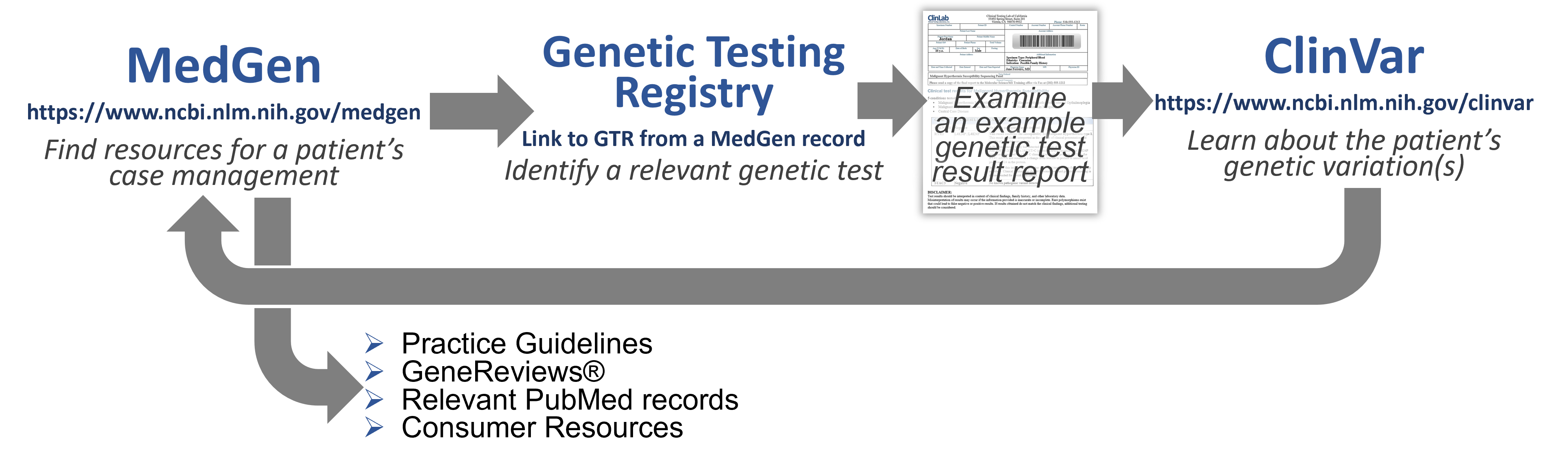
Welcome to Your Patient!
 Jordan, 16 year old male, was referred to you.... Jordan, 16 year old male, was referred to you....Upcoming Procedure: Ross Procedure for stenotic aortic valve replacement Jordan was referred after pre-operative assessment. During your intake interview with Jordan, his mother and aunt, his aunt spoke up and mentioned that her husband (Jordan's uncle) unexpectedly died during "routine surgery". Due to this family history, before her gastric bypass surgery Jordan's mother was scheduled for a muscle biopsy and subsequently tested positive for Malignant hyperthermia. Jordan has been referred to you for genetic testing and his surgery is on hold pending the results. Based on this information, the anesthesia team may choose to alter his care plan. |
(P.S. He's now in his mid-30s and doing well!)
Learn more about Jordan's proposed diagnosis
- To learn more about the proposed diagnosis of Malignant Hyperthermia, search MedGen (https://www.ncbi.nlm.nih.gov/medgen/) with:
 If you need it, you can click here to get to a link for the Medgen record page.
If you need it, you can click here to get to a link for the Medgen record page.
![]() How does this information seem to fit with Jordan's family history?
How does this information seem to fit with Jordan's family history?
Note: To assist you further in learning about this disorder and for preparation for discussions with your patient, there are additional MedGen links to:
-
-
-
-
Relevant publications available in PubMed.
-
Clinical Trials in ClinicalTrials.gov.
-
-
-
3. Let's focus on the preliminary diagnosis of Malignant hyperthermia of anesthesia. Scroll to the Disease Characteristics section and scan the summary Excerpted from the GeneReview to learn more about this disorder.
Note: GeneReviews® is a project run by the University of Washington - producing expert-authored, point-of-care information with clinically relevant and medically actionable information for inherited conditions. It is an incredible review article-type of resource, and is thus featured in it's own section on relevant MedGen records - as an abstract with links to key sections. You should consider accessing and reading the whole article!
 What should you take into consideration before ordering a Genetic Test?
What should you take into consideration before ordering a Genetic Test?
-
-
- Pros
- Genetic tests are decreasing in cost & are not particularly invasive.
- A well-known genetic lesion can sometimes help in diagnosis and/or drug/therapy selection - may provide actionable information.
- A finding may predict disorders before symptoms begin for proactive & preventative care.
- Cons
- We are early in our understanding of genes, gene variants and disease: Failure to detect a pathogenic variant does not rule out the diagnosis.
- Prediction isn’t guaranteed - as pathogenic variants sometimes do not have consistent phenotypic impact in all patients (penetrance, severity, multi-genic & environmental influences).
- Lack of coverage by some insurance companies…
- Pros
-
Find a genetic test to order and examine the results
 If you need it, you can click here to get to a link for the Medgen record page.
If you need it, you can click here to get to a link for the Medgen record page.
4. In the Genetic Testing Registry section of the MedGen record (on the right), click on the See all link to retrieve information on all of the genetic test information that has been submitted to us by providers for this disorder or condition.
Note: The information shown in the NIH Genetic Testing Registry (GTR) is submitted by the testing laboratory. If you have any questions, you should click the "Laboratory Contact" tab for ways to contact them directly
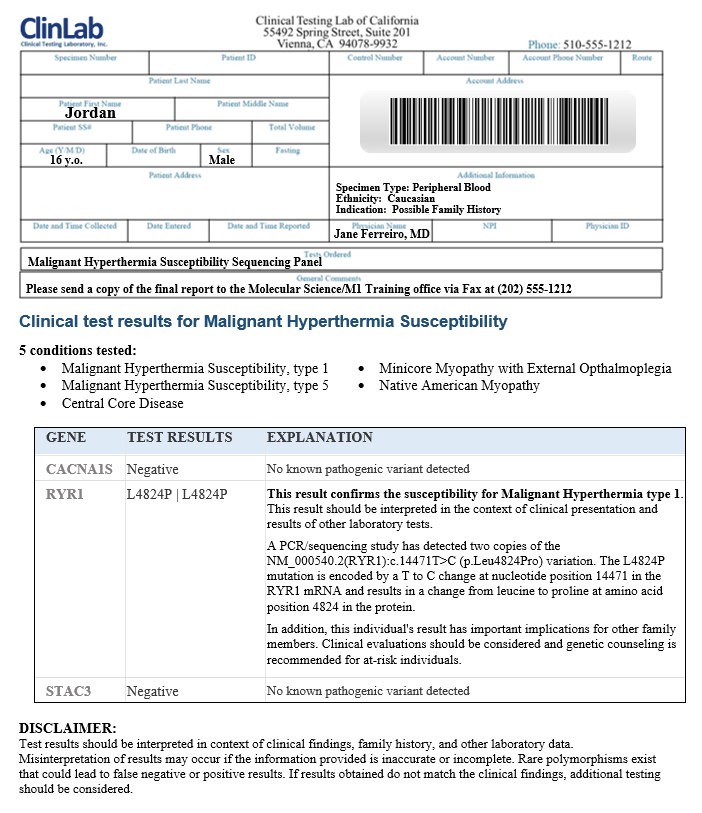
Note: There is currently no established standard format for the results. Each laboratory creates it's own report - some are very detailed, some pretty terse. We are providing you an example format.
 Now that you are a-ground....What to consider when discussing the results of a Genetic Test.
Now that you are a-ground....What to consider when discussing the results of a Genetic Test.
-
-
- Clinically, what do you do with this information?
- Hopefully, you already knew what to do with the information (potential impact of a genetic variant on the patient’s physiology and phenotype and how this relates to your choice of case management) – before the test was ordered.
- A patient may ask: “What is wrong with me and how can we fix it?" A great reason to consult with a Genetic Counselor!
- Outside of this planned clinical event: A patient may ask: “What do I (we) do now?”
- Implications for the patient - beyond this particular surgery: Consider having them discuss this with their primary care physician, dentist, and any other clinical professionals who may need to know for their care.
- Implications for the patient’s family members: Should they tell others?
- Clinically, what do you do with this information?
-
Validate the genetic test result assertion and find more information about a genetic variant
- To validate what is asserted by this clinical testing laboratory, search NCBI’s ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/) with:
 If you need it, you can click here to get to a link for the ClinVar record page.
If you need it, you can click here to get to a link for the ClinVar record page.
![]() What does the ClinVar record indicate in the Clinical Significance field for these genetic variations?
What does the ClinVar record indicate in the Clinical Significance field for these genetic variations?![]() To learn more about them, click the hyperlinked Variation location.
To learn more about them, click the hyperlinked Variation location.
Important! Assertions about the clinical significance or interpretation are provided to NCBI by submitters. All those who have provided information are listed in the Submitted interpretations and evidence section of the record, so that you can look at them all and learn more about what each submitter provided.
![]() Based on the information listed in this section for the RYR1 p.L4824P variant, why do you think ClinVar displays the particular Interpretation term on this record?
Based on the information listed in this section for the RYR1 p.L4824P variant, why do you think ClinVar displays the particular Interpretation term on this record?
![]() In addition to links in the Submitted interpretations and evidence table, the ClinVar record provides additional Citations for this variant - links to key PubMed records as well as other helpful resources such as ClinGen's Evidence Repository (erepo).
In addition to links in the Submitted interpretations and evidence table, the ClinVar record provides additional Citations for this variant - links to key PubMed records as well as other helpful resources such as ClinGen's Evidence Repository (erepo).![]() Keep in mind that the research community is constantly learning new things about genetic variants. Might this particular VUS interpretation change over time? How should/could this be handled?
Keep in mind that the research community is constantly learning new things about genetic variants. Might this particular VUS interpretation change over time? How should/could this be handled?
Find a practice guideline to identify actionable recommendations
 If you need it, you can click here to get to a link for the ClinVar record page.
If you need it, you can click here to get to a link for the ClinVar record page.
Note: Both genetic testing as well as case management gudelines are included in this group of citations.
The simplest statement of how this diagnosis could impact Jordan's care:
European Malignant Hyperthermia Group (EMHG) recommendation: "The most crucial recommendation is that malignant hyperthermia-susceptible patients should receive anaesthesia that is free of triggering agents."
Find Patient Education materials to share with the patient and his family
-
-
- Professional literature such as a the full GeneReviews Chapter on the NCBI Bookshelf, OMIM or one of the Reviews in PubMed.
- For a more lay audience, you could find information in MedlinePlus or MedlinePlus Genetics (GHR) or NIH's NCATS Genetic and Rare Diseases Information Center
-
 You discuss the results of the genetic test and diagnosis with Jordan, his aunt and mother and write a report for the anesthesia team. In addition, you hand Jordan and his family some Patient Education materials and ask them about any questions they may have or things they would like to chat about. You discuss the results of the genetic test and diagnosis with Jordan, his aunt and mother and write a report for the anesthesia team. In addition, you hand Jordan and his family some Patient Education materials and ask them about any questions they may have or things they would like to chat about.The aunt and mother have been and are concerned about the implications of this genetic condition for Jordan and other members of their family. They would like to know what specific things they should be concerned about and avoid and if this condition has ramifications for health-related issues outside of surgical anesthesia, such as Exertional Rhabdomyelitis or Exercise-induced malignant hyperthermia. |
Case Recap
This case study demonstrated how genetic testing can be helpful to identify risks for key disorders that might impact Jordan's peri-operative care.- Case management for the disorder
- For persons diagnosed with pathogenic variants for Malignant Hyperthermia, do not use:
- Halogenated volatile anesthetics, such as enflurane, methoxyflurane, desflurane, halothane, isoflurane, sevoflurane.
- The depolarizing neuromuscular blocker succinylcholine.
- Instead, substitute these drugs:
- Anesthetics such as propofol supplemented by benzodiazepines, opioids, nitrous oxide, or regional anesthetic techniques. Amide and ester local anesthetic agents can also be used in these patients.
- Non-depolarizing neuromuscular blockers such as mivacurium, atracurium, rocuronium, pancuronium, cisatracurium, and vecuronium.
- For persons diagnosed with pathogenic variants for Malignant Hyperthermia, do not use:
- Jordan may want to inform other healthcare practicioners, in case they need to do procedures involving triggering agents, such as his dentist.
- Because of a possible risk for exposure to non-anesthetic triggering conditions, such as Exertional heat stroke or Exertional rhabdomyolysis, Jordan may want to discuss that mid-summer athletic camp with his care team.
Take-away Message!
This case study was an example of how genetic testing for diagnosis of a disorder might impact the optimal case management plan for a particular patient based on their genetics. It also showed that understanding a patient's particular risk may have wide implications for both themselves and their families and could help to inform health and medical care beyond one incident.
Last Reviewed: April 18, 2023

