Exhibition Gallery
Exhibition Gallery
Portrait Gallery
Celebrating America's Women Physicians
Women have always been healers. As mothers and grandmothers, women have always nursed the sick in their homes. As midwives, wise women, and curanderas, women have always cared for people in their communities. Yet, when medicine became established as a formal profession in Europe and America, women were shut out.
Women waged a long battle to gain access to medical education and hospital training. Since then, they have overcome prejudices and discrimination to create and broaden opportunities within the profession. Gradually, women from diverse backgrounds have carved out successful careers in every aspect of medicine.
Changing the Face of Medicine introduces some of the many extraordinary and fascinating women who have studied and practiced medicine.
This 2003 exhibition honors the lives and achievements in medicine. Women physicians have excelled in many diverse medical careers. Some have advanced the field of surgery by developing innovative procedures. Some have won the Nobel prize. Others have brought new attention to the health and well-being of children. Many have reemphasized the art of healing and the roles of culture and spirituality in medicine.
Celebrating America's Women Physicians
Women have always been healers. As mothers and grandmothers, women have always nursed the sick in their homes. As midwives, wise women, and curanderas, women have always cared for people in their communities. Yet, when medicine became established as a formal profession in Europe and America, women were shut out.
Women waged a long battle to gain access to medical education and hospital training. Since then, they have overcome prejudices and discrimination to create and broaden opportunities within the profession. Gradually, women from diverse backgrounds have carved out successful careers in every aspect of medicine.
Changing the Face of Medicine introduces some of the many extraordinary and fascinating women who have studied and practiced medicine.
This 2003 exhibition honors the lives and achievements in medicine. Women physicians have excelled in many diverse medical careers. Some have advanced the field of surgery by developing innovative procedures. Some have won the Nobel prize. Others have brought new attention to the health and well-being of children. Many have reemphasized the art of healing and the roles of culture and spirituality in medicine.
Close Menu ITEM 1 of 0
Dr. Tenley E. Albright
Dr. Tenley Albright became the first American woman to win an Olympic gold medal in figure skating before breaking boundaries in the field of surgery.
Click on the video play button to watch an interview with Dr. Albright.
-
ReadBiography
-
Transcript
Dr. Tenley E. Albright. In 1956 the Olympics was in Cortina, Italy, in the mountains, and we skated outdoors. It’s sort of a hyper-sensation, hyper-perception, you’re able to think of many, many things at once. I was aware of so many things. Of the people in the audience, about where I was standing, where the sun was crossing the ice, where I’d take off in the dark and land in the sun, what the mountains looked like, what the moment was. And so when you’re there in this magical world of the operating room, with a patient and with a team, and you’re dealing with something, you never know totally what you’re going to find until you’re there. It’s sort of like that multidimensional thinking that I was aware of on the ice, where everything comes into your head at once. You have to be focused, but you also have to be conscious of all sorts of things, for the benefit of having the surgery turn out the way you want it to. Doing whatever I can to make a difference in one life, or part of one life, that motivates me to want to do that more. And anything I can do to make a bigger change—whether it’s helping to change attitudes or ways of doing things or just to encourage all of us to have sort of a sense of openness— that’s really what I’d like to do.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Mary Ellen Avery
Dr. Mary Ellen Avery helped discover the cause of respiratory distress syndrome (RDS) in premature babies. Additionally, she trained and advocated for young physicians in a long career in academic medicine.
Click on the video play button to watch an interview with Dr. Avery.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Mary Ellen Avery. My next door neighbor was professor of pediatrics at Woman’s Medical College in Pennsylvania—Dr. Emily Bacon— and she kindly reached out to me in many ways, and I saw her life as more exciting and meaningful than most of the women I knew—who were my mothers friends, for example, who were busy doing good works, raising children (and I admired them greatly), but I still thought Emily Bacon had something going for her in terms of reaching out to all children. But mainly, she reached out to me, and I’m eternally grateful. So I applied to Johns Hopkins and Harvard. And Harvard didn’t take women at that time but I didn’t know it, and Johns Hopkins did. In fact they had to. They were founded by a woman who had insisted that they wouldn’t get the money to build the school if they didn’t take women on an equal basis with men, and I thought, “Hey, that neutralizes the problem in one dimension,” and Emily Bacon graduated from Johns Hopkins. So there was no question where I was going to go to medical school. I received the National Medal of Science in 1991. It is America’s highest award for all of science. And so there had been very few pediatricians if any, that had ever been given the medal. They’ve given maybe ten or fifteen a year. It’s presented by the President of the United States to the nominee. This has been very, very rewarding. And I feel that I am a citizen of this one world and that I can resonate with people with a lot in common—it’s called science and science methods. And I am so saturated and pleased to share it with anybody who will listen, and that makes for a very fulfilling life.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Nancy E. Jasso
Dr. Nancy Jasso is one of the founding physicians of a laser tattoo–removal project for the San Fernando Valley Violence Prevention Coalition, which serves people who leave gangs.
Click on the video play button to watch an interview with Dr. Jasso.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Nancy E. Jasso. For many people with tattoos, it’s actually life threatening to them to walk the streets. If they happen to have the wrong tattoo in the wrong neighborhood, then that means they might get shot, and they may not make it to the next day. In addition, it’s very difficult for them to secure employment when they have tattoos. There’s lots of value judgments about having tattoos, lots of concern for safety, and what their affiliations might be with either gangs or drugs, and so many people cannot get employed if they have tattoos. I have a lot of respect for the patients in the Tattoo Clinic. These are patients who are really trying to change their lives, and change is hard. And yet they’ve been courageous enough to actually try to put their life on a different track. So I figure anything that I can do to be helpful to them, I'm very willing to do. Well, I think fundamentally, being a physician is really an honor. It’s really a privilege to walk that path with another human being. People come in because they’re suffering and they’re in need of help, and I have the privilege of being there to try to assist them. And I really do see it like a partnership. It’s not really a one-way street. I certainly have my bag of tricks and all of the years of study under my belt, but it really takes kind of the two of us working together to really come up with something that’s going to help them.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Vivian W. Pinn
Dr. Vivian Pinn served as the first full–time director of the Office of Research on Women’s Health (ORWH) at the National Institutes of Health (NIH). Additionally, she was the first African American woman to chair an academic pathology department in the United States, at Howard University College of Medicine.
Click on the video play button to watch an interview with Dr. Pinn.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Vivian W. Pinn. Having the opportunity to come be the first permanent Director of the Office of Research on Women’s Health at the National Institutes of Health (NIH) represented not only a career change for me, but also a very, very exciting opportunity that I have tried to make the best of in every way that I could. We didn’t really have a good focus on what is now called Women’s Health up until about the time this office was established. The office at NIH is really the first office established within the Federal Government to focus on women’s health issues. It was established to make sure that women are included in clinical studies funded by the NIH—in other words, included in research—and to make sure that research is addressing the health of women in studies. I always wanted to be a physician and I always thought that was what I wanted to do. But my sophomore year in college, my mother developed a bad pain in her back. And the doctors thought it was arthritis. And I can remember going with her to the doctor and having him say, “Francina, if you just wore those oxfords I gave you and stood up straight and did those exercises, you wouldn’t have that pain.” But it turned out what he had missed, was that she had a bone tumor. I interrupted my career and stayed home with my mother and took care of her 24 hours a day until she died, which was in February of 1961. Then I went back to school with even more resolve that I wanted to be a physician, and I wanted to be the kind of physician who paid attention to my patients, and didn’t dismiss my patient’s complaints—something that has really carried through and I think has been central to my way of thinking and approaching women’s health in this portion of my career.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Esther M. Sternberg
Dr. Esther Sternberg is internationally recognized for her groundbreaking work on the mind–body connection in illness and healing.
Click on the video play button to watch an interview with Dr. Sternberg.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Esther M. Sternberg. It’s really hard to say “Okay, I’ve made a discovery, and I know I’ve helped thousands of people, or millions of people.” It’s when you see the one patient that really has benefited from that discovery that you really know that you’ve helped. When the family member can come up to you and say, “Thank you, you helped save my mother.” That really makes a difference. And I think that’s what motivated me from the beginning when I started seeing patients on a one-on-one basis, when you know that you’ve saved a life. And then if you make a discovery in the lab, in a rat, that you know can be applied to saving many lives — that really is tremendously rewarding. For so many thousands of years, the popular culture believed that stress could make you sick, that believing could make you well. And people believe what they feel. But scientists need evidence. And there really wasn’t any good, solid scientific evidence to prove these connections. Nor was there a good way to measure them. And scientists only believe what they can actually measure. Once scientists and physicians believed that there was a connection between the brain and the immune system, you could then take it to the next step: that maybe there is a connection between emotions and disease. Between negative emotions and disease, and positive emotions and health. And we can then say, okay, maybe these alternative approaches that have been used for thousands of years — approaches like meditation, prayer, music, sleep, dreams — all of these approaches that we really know in our heart of hearts really work to maintain health... Maybe there is a scientific basis for it.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Donna M. Christian-Christensen
Dr. Donna Christian–Christensen is the first woman physician to serve in Congress and the first woman delegate for the U.S. Virgin Islands.
Click on the video play button to watch an interview with Dr. Christian–Christensen.
-
ReadBiography
-
Transcript
Dr. Donna M. Christian-Christensen. If you had asked me when I was graduating from George Washington in 1970 if I would be here doing this, I would have said no. And if you had asked me in 1996, when I got elected, if I would be in a position to influence national health issues, or international health issues, I would have told you, “Oh, no, that wasn’t possible,” but today it is. And it’s really an honor and a privilege, and a responsibility, to be able to do that. Starting coalitions is a lot of work. You end up doing all of it yourself. So I thought, well let me see, maybe I could join an organization that already exists that I could work through, and do some of the same kinds of things. And so I ended up joining the Democratic Party. And I was the first female delegate from the U.S. Virgin Islands— the first female delegate from any of the territories as a matter of fact—and then the first female physician ever to serve in the Congress. I think it’s really important for young people of color to see people of their own racial or ethnic background in positions like mine—not only on the political front, but also as a health care provider—so that they will know that yes, it’s possible for them. Because sometimes in their day-to-day environment it may not seem that way. So I think it’s really encouraging for them to see us and to interact with us.
-
Copy Link
Copied
Close Menu ITEM 1 of 0
Dr. Nancy L. Snyderman
Dr. Nancy Snyderman had a decades’ long career in broadcast medical journalism, serving as a correspondent for ABC television’s Good Morning America for 15 years.
Click on the video play button to watch an interview with Dr. Snyderman.
-
ReadBiography
-
Transcript
Dr. Nancy L. Snyderman. No matter where I have been at any stage of my life I’ve always been a doctor first, and everything else second— except maybe being a mom. But I’ve never seen myself as a doctor correspondent who just happens to do surgery. I’ve always defined myself as a practicing surgeon who happens to also have a second career in broadcast journalism. I started combining my love of television with my love of medicine. And the two weaved themselves together quite well. The passion in broadcasting is different. The best stuff I’ve done has been in the worst places on earth. Kosovo. Mogadishu. Bosnia. The Persian Gulf. Afghanistan. Pakistan. I think when you get a chance to look around you and see the world suffering, and you’ve reached down deep inside yourself and tried to explain that to people who may never have the good fortune to travel, in the same way, that’s where I get my passion. And if you look at the people entering medicine today, they’re as bright as people have ever been. The youngsters entering medicine today will enter on their own terms. And they’ll make medicine what they want it to be. But I want young people—particularly young girls—to discover the thrill of science, and biology, and physics, and how it all works. And for my two girls, every time we can draw science or biology into life, we do it. Medicine’s filled with a lot of kicks. And the other great thing is, it’s this blank canvas. You want to go into medicine? You get to do anything you want to do. Become a neuropsychiatrist, become a physicist, become a neurosurgeon, be in the lab, see patients, work part-time, full-time, have kids, don’t have kids— you get to do it on your own terms. It’s great. And you can always put food on the table.
-
Copy Link
Copied
Setting Their Sights
Before women could build careers as physicians, they had to fight even to be allowed to attend medical school. After proving that they were as capable as men, they went on to campaign for additional professional training and other career opportunities.
As part of the wider movement for women’s rights during the mid–1800s, women campaigned for admission to medical schools and the opportunity to learn and work alongside men in the professions. Such rights came slowly. Even after qualifying as physicians, women were often excluded from employment in medical schools, hospitals, clinics, and laboratories.
To provide access to these opportunities, many among the first generation of women physicians established women’s medical colleges or hospitals for women and children.
Persistence, ingenuity, and ability enabled women to advance into all areas of science and medicine. Courageously, they worked long and hard to succeed even where they were most unwelcome, such as in surgery and scientific research.
Setting Their Sights
Opening Doors
The first women to complete medical training and launch careers confronted daunting professional and social restrictions. To establish their rightful place as physicians and to expand opportunities for other women in medicine, they devised many strategies, establishing their own hospitals, schools, and professional societies. They excelled in their chosen fields of medical practice and scientific research—often while campaigning for political change and managing the administrative responsibilities and financial affairs of educational and medical institutions.
By succeeding in work considered “unsuitable” for women, these leaders overturned prevailing assumptions about the supposedly lesser intellectual abilities of women and the traditional responsibilities of wives and mothers.

Close Menu ITEM 0 of 0
Dr. Elizabeth Blackwell
When she graduated from New York’s Geneva Medical College, in 1849, Elizabeth Blackwell became the first woman in America to earn the M.D. degree. She supported medical education for women and helped many other women’s careers. By establishing the New York Infirmary in 1857, she offered a practical solution to one of the problems facing women who were rejected from internships elsewhere but determined to expand their skills as physicians. She also published several important books on the issue of women in medicine, including Medicine as a Profession For Women in 1860 and Address on the Medical Education of Women in 1864.
The Schlesinger Library, Radcliffe Institute, Harvard University
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Mary Corinna Putnam Jacobi
Mary Putnam Jacobi was an esteemed medical practitioner and teacher, a harsh critic of the exclusion of women from the professions, and a social reformer dedicated to the expansion of educational opportunities for women. She was also a well–respected scientist, supporting her arguments for the rights of women with the scientific proofs of her time.
Library of Congress, Prints and Photographs Division, LC–USZ62–61783
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
-

Gathering Data
Before the sphygmograph was developed, physicians assessed pulse strength by placing their fingers on a patient’s wrist and feeling for arterial resistance. The sphygmograph offered a more consistent method to assess, compare, and present information about the strength of the pulse. Dr. Mary Putnam Jacobi used the device in her research.
National Library of Medicine
-
ReadBiography
-
EnlargeImage
-
Transcript
Gathering Data Before the sphygmograph was developed, physicians assessed pulse strength by placing their fingers on a patient’s wrist and feeling for arterial resistance. The sphygmograph offered a more consistent method to assess, compare, and present information about the strength of the pulse. Dr. Mary Putnam Jacobi used the device in her research. Screw recording. Stylus. smoked paper transporter. smoked paper. pressure sensor. ivory rests. pressure dial. clockwork mechanism.
-
Copy Link
Copied
-
-

Mahomed sphygmograph, ca. 1880
A number of sphygmographs (instruments to measure and record the force of the pulse) were developed during the 19th century. The one shown here was designed during the 1870s by medical student F. A. Mahomed. One end of a metal stylus was strapped to the subject’s wrist, allowing the pressure of the pulse through an artery to move the other end of the stylus, tracing a record across sliding, smoke–blackened paper.
M. Donald Blaufox, M.D., Ph.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
Dr. Jacobi's Sphygmograph

Close Menu ITEM 3 of 0
Dr. Emily Dunning Barringer
Emily Dunning Barringer harnessed the benefits of a good education and gained the mentorship of a leading woman physician of her era, Dr. Mary Putnam Jacobi, to overcome barriers in her own career and to make it possible for other women physicians to serve their country during World War II. After first being denied an appointment at New York’s Gouverneur Hospital, she was later allowed to take up the position and became the hospital’s first woman medical resident and ambulance physician. During World War II, Barringer lobbied Congress to allow women physicians to serve as commissioned officers in the Army Medical Reserve Corps, and in 1943 the passing of the Sparkman Act granted women the right to receive commissions in the army, navy, and Public Health Service.
New York Times Archive
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 4 of 0
Dr. Emily Dunning Barringer
Dr. Emily Dunning Barringer became the first woman medical resident and ambulance physician in New York. She also lobbied Congress to allow women physicians to receive commissions in the Armed Forces and the Public Health Service.
Click on the video play button to watch a video on Dr. Dunning Barringer.
-
ReadBiography
-
Transcript
Dr. Emily Dunning Barringer became the first woman to ride with ambulance crews as an emergency physician, in New York City, working from a horse-drawn wagon in the neighborhoods of the Lower East Side. Originally, Emily Dunning thought she would become a nurse. It was Dr. Mary Putnam Jacobi who recommended Cornell University’s medical preparatory course for her education instead. Dr. Jacobi believed Emily Dunning would choose to become a doctor. In 1897 she enrolled at the College of Medicine of the New York Infirmary. The day after she completed her residency, in 1904, she married Dr. Benjamin Barringer. Quickly, she became frustrated that his prospects were so much better than hers. She said, “He could count on a splendid training in one of the big general hospitals... with post-graduate work abroad, in whatever line he elected... And I? What did I see ahead?” Her opportunities seemed greatly limited. Again, Dr. Mary Putnam Jacobi advised Dr. Barringer, urging her to take the competitive internship exams held by New York’s large area hospitals even though women had never been allowed to compete. Together, the two women pressured several hospitals to open their internships to women. Dr. Barringer became the first woman medical resident at Gouverneur Hospital in New York City. Her male colleagues harassed her assigning her difficult schedules for on-call and ward duties. She continued with her work, despite these difficult circumstances and was widely reported in the local papers as something of a novelty as a woman ambulance physician. During World War II, Dr. Barringer made headlines again, lobbying Congress for military commissions for women physicians. While women could serve as contract surgeons in the Women’s Army Auxiliary Corps, they were not commissioned employees, and so were not given the same benefits as men. In 1943, the Sparkman Act was signed into law, allowing women the same benefits as men in the Army and Navy. Dr. Emily Dunning Barringer created a legacy of helping women achieve equal status, in the medical profession, and in the U.S. military; Opportunities passed on to the generations to come.
-
Copy Link
Copied

Close Menu ITEM 5 of 0
Dr. Marie E. Zakrzewska
In 1862, Marie Zakrzewska, M.D., opened doors to women physicians who were excluded from clinical training opportunities at male–run hospitals, by establishing the first hospital in Boston—and the second hospital in America—run by women, the New England Hospital for Women and Children.
Sophia Smith Collection, Smith College
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 6 of 0
Dr. Marie E. Zakrzewska
Dr. Marie Zakrzewska founded the New England Hospital for Women and Children, the second hospital in the United States to be run by women physicians and surgeons.
Click on the video play button to watch a video Dr. Zakrzewska.
-
ReadBiography
-
Transcript
Dr. Marie E. Zakrewska In 1862, Dr. Marie Zakrzewska opened her own hospital, The New England Hospital for Women and Children. It was the first hospital in Boston, and only the second in America to be run by women physicians. Dr. Zakrzewska had been part of the first generation of women physicians in America. Barred from working in existing hospitals and excluded from teaching jobs at medical schools, some of these women went on to found dispensaries, hospitals, and schools to train women students and employ women physicians. Marie Zakrzewska was born in Berlin, the daughter of a midwife. As a young woman, she accompanied her mother on her rounds. She trained at the Royal Charité Hospital, and in 1852 become a midwife. When her promotion to Head Midwife not long after she had finished her training was met with disapproval from some of the faculty, she left to study medicine in the United States. Although opportunities in America were also limited, Marie Zakrzewska was aided by Dr. Elizabeth Blackwell, the first woman to graduate from medical school in America. With Dr. Blackwell’s help, she enrolled at Cleveland Western Reserve College, traditionally, an all-male medical school. Marie Zakrzewska was one of only six women admitted to the school in the 1850s. She graduated with her M.D. in 1856. Dr. Blackwell and her sister Emily became an inspiration to Dr. Zakrzewska by planning to found a small hospital where women physicians could work and learn. Dr. Zakrzewska joined their effort, and the New York Infirmary for Women and Children opened in 1857. She served as resident physician at the hospital for two years. She moved to Boston to accept the position of Professor of Obstetrics at the New England Female Medical College. Her students, encountering the same obstacles as other women physicians, found it difficult to get work after graduation. Dr. Zakrzewska also disagreed with the founder of the New England Female Medical College over the school’s curriculum. She had proposed courses in dissection and microscopy to enhance the training of students and keep up with the developing field of scientific medicine. But the director intended to limit women physicians to a lower educational level. Three years later, she resigned, to open her own hospital. The New England Hospital for Women and Children flourished under Dr. Zakrzewska’s direction. There, women physicians who were excluded from the majority of hospitals, could acquire clinical experience. She believed that women physicians must have the same training and base of scientific knowledge as their male counterparts to achieve the same levels of research and standards of practice.
-
Copy Link
Copied

Close Menu ITEM 7 of 0
Dr. Ann Preston
As the first woman to be made dean of the Woman's Medical College of Pennsylvania (WMCP), Ann Preston campaigned for her students to be admitted to clinical lectures at the Philadelphia Hospital, and the Pennsylvania Hospital. Despite the hostility of the all–male student groups, she was determined to negotiate the best educational opportunities for the students of WMCP.
National Library of Medicine, Images from the History of Medicine, B030140
-
ReadBiography
-
DigitalCollections
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 8 of 0
Dr. Ann Preston
Dr. Ann Preston was the first woman dean of the Woman’s Medical College of Pennsylvania and advocated for women students to receive medical education.
Click on the video play button to watch a video on Dr. Preston.
-
ReadBiography
-
Transcript
Dr. Ann Preston In 1869, Dr. Ann Preston, the first woman Dean of the Woman’s Medical College of Pennsylvania, campaigned for the right for her students to attend lectures at all-male institutions. When they were first granted admittance, women medical students attending a clinic were greeted by the male students with hisses and paper wads. Dr. Preston refused to be deterred, and successfully argued for the fair treatment and equal skill of her students. She was born a Quaker in 1813, and attended Quaker schools in Pennsylvania. From an early age, she campaigned for social reform. She wrote petitions and lectures for the Clarkson Anti-Slavery Society and joined the temperance movement. Wanting to educate women about their own bodies, she began teaching physiology and hygiene to all-female classes. In 1847, Ann Preston applied to four medical colleges in Philadelphia. But her applications, like those from all other women, were rejected. To provide opportunities for women to study medicine, a group of Quakers founded the Woman’s Medical College of Pennsylvania. Ann Preston enrolled in the first class. She graduated in 1851, at the age of 38. She stayed on at the school, and in two years was appointed professor of physiology and hygiene. Public and professional attitudes toward women physicians remained negative, for the most part. Eight years after the medical school was established, the Philadelphia Medical Society spoke out against it, effectively barring women students from educational clinics and medical societies in the city. Undeterred, Dr. Ann Preston organized a board of wealthy supporters to fund and run a woman’s hospital, where her students could gain clinical experience. The hospital opened in 1861. Two years later, Dr. Preston established a School of Nursing. In 1865, Dr. Ann Preston became the first woman Dean of the Woman’s Medical College. Committed to expanding her students’ educational opportunities, Dr. Preston negotiated and won the right for them to attend general clinics at the Blockley Hospital in Philadelphia. In 1869, she made a similar arrangement with the Pennsylvania Hospital. There, the women endured harassment from the male students. As one student later recalled, “We were allowed to enter by way of the back stairs, and were greeted by the male students with hisses and paper wads, and frequently during the clinic were treated to more of the same... The Professor of Surgery came in and bowed to the men only...” Dr. Ann Preston publicly criticized the response of the men and the attitudes behind it, arguing that women students could easily keep up with the men but that the men refused to welcome their equally capable women colleagues. Thanks to Dr. Preston and her students, women studying alongside men gradually became a more frequent sight in the medical clinics and colleges of the late 1800s.
-
Copy Link
Copied

Close Menu ITEM 9 of 0
Dr. Sarah Reed Adamson Dolley
Sarah Adamson Dolley of Rochester, New York, was the first woman physician to complete a hospital internship. She was a founder of one of the first general women’s medical societies, the Practitioners’ Society of Rochester, New York, and the Provident Dispensary for Women and Children (an outpatient clinic for the working poor) established by the society. She was also the first president of the Women’s Medical Society of New York State.
Edward G. Miner Library, Rochester New York
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 10 of 0
Dr. Sarah Reed Adamson Dolley
Dr. Sarah Adamson Dolley was the third woman medical graduate in the United States and the first woman to complete a hospital internship.
Click on the video play button to watch a video on Dr. Dolley.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Sarah Read Dolley Sarah Read Adamson was born in 1829 and became the third woman in America to earn an M.D. degree. Her family were Quakers living in Schuykill Meeting, Chester County, Pennsylvania. She was educated at The Friends’ School in Philadelphia. Sarah Adamson became interested in medicine when her teacher, Graceanna Lewis, gave her a physiology book to study at home. Her uncle, Hiram Corson, was a physician, and she had also read an anatomical book from his library. He agreed to tutor her, and took her on as an apprentice. This experience prepared her to study at the newly-opened Central Medical College in Rochester, New York, where she graduated from in 1851. Though a few women had broken through barriers to receive a medical education, no woman had ever completed a hospital internship. Dr. Adamson’s uncle again supported her, sponsoring her application for an internship at Blockley Hospital in Philadelphia. She became the first woman intern in America. In 1852, she married Dr. Lester Clinton Dolley, a professor of anatomy and surgery at Central Medical College. Together they traveled to Europe to gain further medical training, attending clinics in Paris, Prague, and Vienna. Upon their return, they set up a medical practice in Rochester, where they worked together until his death in 1872. For the next year, Dr. Sarah Dolley served as Professor of Obstetrics at the Woman’s Medical College of Pennsylvania, but soon returned to Rochester to re-establish her practice. Women were still barred from working in most hospitals. Knowing how critical the knowledge and experience she had gained through her internship was, Dr. Dolley worked to open more hospital positions to women. In 1887, she helped a group of women open their own dispensary, an outpatient clinic for the working poor. She also helped found one of the first general women’s medical societies: The Practitioners’ Society of Rochester, which later became the Blackwell Society. On her seventy-eighth birthday, Dr. Sarah Adamson Dolley led the Blackwell Society in launching the Women’s Medical Society of the State of New York. She was given the honor of being its first president.
-
Copy Link
Copied

Close Menu ITEM 11 of 0
Dr. Mary Amanda Dixon Jones
Dr. Mary Dixon Jones became a world–renowned surgeon for her treatment of diseases of the female reproductive system, in a time when few women physicians were able to build a career in the specialty. She is credited as the first person in America to propose and perform a full hysterectomy (surgical removal of the uterus) for the treatment of uterine myoma (a tumor of muscle tissue). She trained with Mary Putnam Jacobi in New York and is considered one of the leading women scientists of the late nineteenth century.
Courtesy of the New York Academy of Medicine Library, copy by RD Rubic
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 12 of 0
Dr. Mary Amanda Dixon Jones
Dr. Mary Amanda Dixon Jones was a renowned surgeon credited as the first person to propose and perform a full hysterectomy to treat a tumor in uterine muscle tissue.
Click on the video play button to watch a video on Dr. Dixon Jones.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Mary Amanda Dixon Jones In 1888, Dr. Mary Dixon Jones performed a hysterectomy, removing a seventeen-pound tumor from her patient’s uterus. It was the first operation of its kind performed in America. Mary Dixon began her career as an apprentice to two leading male physicians. In 1854, she married a lawyer, John Quincy Adams Jones. They moved west to Illinois and Wisconsin, and had three children. In 1862, ten years after she had first begun studying medicine as an apprentice, Dixon Jones left to study at the Hygeio-Therapeutic Medical College in New York. After graduation, she moved to Brooklyn to start a private practice. Dr. Dixon Jones focused on obstetrical and gynecological surgery, a specialty that was developing rapidly at the time. She read about newly developed, innovative operations described in medical literature. She heard about new techniques taught in medical schools. But some of her patients had complicated and distressing gynecological problems that she was unsure how to treat. So, after ten years of successful private practice, she went back to school, enrolling at the Woman’s Medical College of Pennsylvania. She also studied with Dr. Mary Putnam Jacobi, to discover more about the latest in pathology and clinical diagnosis. After her graduation in 1875, she returned to private practice. For nine years, she also worked at the Woman’s Hospital of Brooklyn. Dr. Dixon Jones’ surgical skills and her use of innovative procedures earned her an impressive reputation and a successful practice. In 1888, she described her precedent-setting hysterectomy surgery in The New York Medical Journal, noting that within fifteen days of the surgery, the patient was almost fully recovered. In 1895, a Brooklyn newspaper slandered her surgical work. Dr. Dixon Jones sued for libel, but lost the case. As a result, her practice dwindled and she was forced to retire, so she turned to research. She studied diseases of the reproductive system and investigated the connections between surgical specimens under the microscope and many of the diseases she had treated. She was one of the few gynecological surgeons of her time to take up the laboratory study of specimens.
-
Copy Link
Copied
Setting Their Sights
Challenging Racial Barriers
The first women of color who gained access to medical school confronted financial hardships, discrimination against women, and racism. For generations, their families had been enslaved or oppressed. They had been denied the means of making a living and access to decent medical care. Even to begin training, these women often had to work their way through medical school or seek funding from supporters of women’s and minorities’ rights.
Once they became doctors, these women played an important role in bringing better standards of care to their own communities and served as role models for other women.

Close Menu ITEM 0 of 0
Dr. Matilda Arabella Evans
Matilda Arabella Evans, who graduated from the Woman’s Medical College of Pennsylvania (WMCP) in 1897, was the first African-American woman licensed to practice medicine in South Carolina. Evans’s survey of black school children’s health in Columbia, South Carolina, served as the basis for a permanent examination program within the South Carolina public school system. She also founded the Columbia Clinic Association, which provided health services and health education to families. She extended the program when she established the Negro Health Association of South Carolina, to educate families throughout the state on proper health care procedures.
South Caroliniana Library, University of South Carolina, Columbia
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 1 of 0
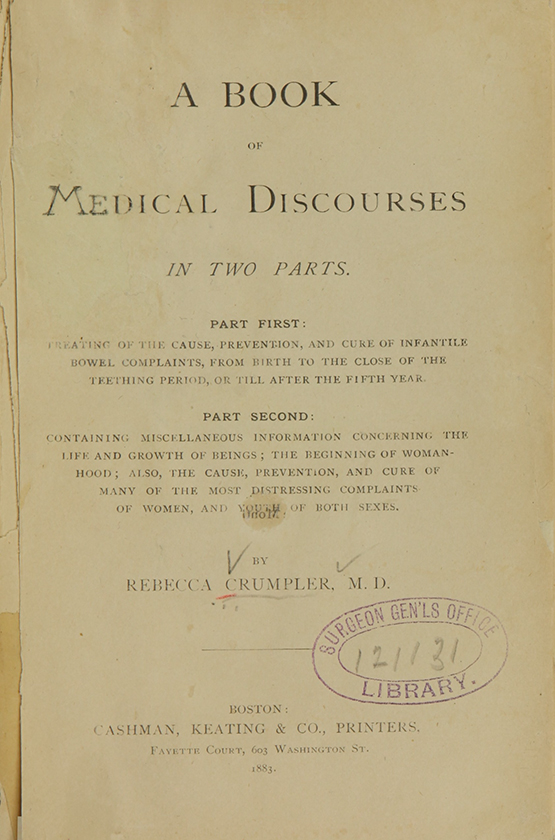
Dr. Rebecca Lee Crumpler
Rebecca Lee Crumpler challenged the prejudice that prevented African Americans from pursuing careers in medicine to became the first African American woman in the United States to earn an M.D. degree, a distinction formerly credited to Rebecca Cole. Although little has survived to tell the story of Crumpler’s life, she has secured her place in the historical record with her book of medical advice for women and children, published in 1883.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Dr. Susan La Flesche Picotte
Susan La Flesche Picotte was first person to receive federal aid for professional education, and the first American Indian woman in the United States to receive a medical degree. In her remarkable career she served more than 1,300 people over 450 square miles, giving financial advice and resolving family disputes as well as providing medical care at all hours of the day and night.
Susan La Flesche, early 1900s, when she returned to the Omaha Reservation
Nebraska State Historical Society Photograph Collections
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 3 of 0
Dr. Rebecca J. Cole
In 1867, Rebecca J. Cole became the second African American woman to receive an M.D. degree in the United States (Rebecca Crumpler, M.D., graduated from the New England Female Medical College three years earlier, in 1864). Dr. Cole was able to overcome racial and gender barriers to medical education by training in all–female institutions run by women who had been part of the first generation of female physicians graduating mid–century. Dr. Cole graduated from the Woman’s Medical College of Pennsylvania in 1867, under the supervision of Ann Preston, the first woman dean of the school, and went to work at Elizabeth Blackwell’s New York Infirmary for Women and Children to gain clinical experience.
National Library of Medicine
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 4 of 0
Dr. Rebecca J. Cole
Dr. Rebecca J. Cole was the first African American woman to receive an MD in the United States.
Click on the video play button to watch a video on Dr. Cole.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Rebecca J. Cole Sadly, as is the case with many records of the achievements of African Americans of her generation, no images have survived of Dr. Rebecca J. Cole. She was the second African American woman to receive an M.D. degree in the United States, in 1867. Rebecca Cole was born and raised in Philadelphia. She completed her secondary education at the first co-educational high school for African Americans in the city. She enrolled at the Woman’s Medical College of Pennsylvania near the end of the Civil War. She trained with Dr. Ann Preston, the first woman dean of the school, and in 1867, was the first African American to graduate. Dr. Cole, like many of her fellow women students of medicine was able to continue her training by joining an institution founded for women patients and practitioners. To gain clinical experience, she took a job at the New York Infirmary for Women and Children, established by physicians Elizabeth Blackwell and her sister Emily, with the help of Dr. Marie Zakrzewska. Dr. Elizabeth Blackwell assigned Dr. Cole the role of health visitor in the local community. She was responsible for dispensing practical advice to mothers living in poverty about the best ways to keep their families healthy. Dr. Blackwell thought Dr. Cole had the ideal character for such work, and mentioned in her autobiography that she had “carried on this work with tact and care.” Dr. Rebecca Cole practiced in South Carolina for a number of years, before returning to Philadelphia. In 1873, she opened a Women’s Directory Center to provide medical and legal services to women and children in need. In January 1899, Dr. Cole was appointed superintendent of a home in Washington, D.C. run by the Association for the Relief of Destitute Colored Women and Children. In her years of caring for families living interrible poverty in the city of Washington, she was most appreciated for the difference she was able to make. As mentioned in one of the annual reports from the association:"Dr. Cole herself has more than fulfilled the expectations of her friends. With a clear and comprehensive view of her wholefield of action, she has carried out her plans with the good sense and vigor which are a part of her character."
-
Copy Link
Copied

Close Menu ITEM 5 of 0
Dr. Helen Octavia Dickens
In 1950, Dr. Helen Dickens was the first African American woman admitted to the American College of Surgeons. The daughter of a former slave, she would sit at the front of the class in medical school so that she would not be bothered by the racist comments and gestures made by her classmates. By 1969, she was associate dean in the Office for Minority Affairs at the University of Pennsylvania, and within five years had increased minority enrollment from three students to sixty–four.
National Library of Medicine, Images from the History of Medicine, B07139
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 6 of 0
Dr. Helen Octavia Dickens
Dr. Helen Dickens was the first African American woman admitted to the American College of Surgeons. She served communities with limited access to health care, provided sex education to women living in poverty, and worked as a professor of surgery.
Click on the video play button to watch a video on Dr. Dickens.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Helen Octavia Dickens Dr. Helen Dickens began her medical career by providing care to those who had no means to obtain treatment. Once, as she visited a house without electricity, she had to drag a bed to the window to deliver a baby by the light from the streetlight outside. Because her parents had struggled to make a living in low-paying jobs, they insisted that their daughter receive a good education. She attended a desegregated high school, applied to the best schools and hospitals and was not intimidated by the idea of training at predominantly white schools. In 1934, when she earned her M.D. from the University of Illinois, Dr. Helen Dickens was the only African American woman in her class. She completed her internship at Provident, a black hospital on the south side of Chicago. Working among the poor, she treated tuberculosis and provided obstetric and gynecological care. Moving to Philadelphia, Dr. Dickens worked for six years at Aspiranto Health Home, treating patients living in poverty, with little access to medical care. To expand her training in obstetrics and gynecology, she returned to Provident Hospital in Chicago. In 1943, she married a fellow resident, Dr. Purvis Sinclair Henderson. They moved to New York City and Dr. Dickens began a residency at Harlem Hospital. She left to get a Master of Science degree from the University of Pennsylvania, then returned to complete her residency at Harlem in 1946. Four years later, Dr. Helen Dickens became the first African American woman to be named a Fellow of the American College of Surgeons. Throughout her career, Dr. Dickens focused on the problems she had seen in her obstetrics and gynecology practice. She wanted to educate young women to give them the knowledge to control their fertility and sexual health. Her extensive research resulted in intervention strategies to help schools, parents, and health professionals reduce the incidence of teen pregnancies, and sexually transmitted diseases. Moving back to Philadelphia, Dr. Dickens taught at the University of Pennsylvania. In 1969, she was appointed Dean of the Office for Minority Affairs. In that role, she reached out to minority students to encourage them to pursue medical careers. Thanks largely to her efforts, minority student enrollment increased from just three students to sixty-four within five years. In 1985, Dr. Helen Dickens was named Professor Emeritus.
-
Copy Link
Copied

Close Menu ITEM 7 of 0
Dr. Eliza Ann Grier
Eliza Ann Grier was an emancipated slave who faced racial discrimination and financial hardship while pursuing her dream of becoming a doctor. To pay for her medical education, she alternated every year of her studies with a year of picking cotton. It took her seven years to graduate. In 1898, she became the first African American woman licensed to practice medicine in the state of Georgia, and although she was plagued with financial difficulties throughout her education and her career, she fought tenaciously for her right to earn a living as a woman doctor.
Archives and Special Collections on Women in Medicine, Drexel University College of Medicine
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 8 of 0
Dr. Eliza Ann Grier
Dr. Eliza Ann Grier was the first African American woman licensed to practice medicine in the state of Georgia.
Click on the video play button to watch a video on Dr. Grier.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Eliza Ann Grier Dr. Eliza Ann Grier had once been a slave. She went on to become the first African American woman licensed to practice medicine in the state of Georgia. After emancipation, Eliza Grier decided to become a teacher, studying for seven years at Fisk University in Nashville, Tennessee. But she aspired to a career as a physician, believing she could be of most benefit to others and earn a fair wage if she had a medical education. “When I saw colored women doing all the work in cases of accouchement ... or, childbirth and all the fee going to some white doctor who merely looked on, I asked myself why should I not get the fee myself.” So, in December of 1890, Eliza Grier wrote to the Woman’s Medical College of Pennsylvania. “I have no money and no source from which to get it,” she wrote, “Only as I work for every dollar.” She asked the dean “if there was any possible way for an emancipated slave to receive any help into so lofty a profession.” She was admitted, but to pay the tuition, Eliza Grier alternated each year of study with a year of picking cotton. Despite these hardships, she did not lose sight of her goal. After seven years of work and study, she graduated in 1897, and returned to Atlanta. Later that year, Dr. Eliza Ann Grier became the first African American woman licensed to practice medicine in the state of Georgia. After only four years, Dr. Grier fell ill and was unable to maintain her medical practice. Determined to keep up with her work, she called on various supporters for help. She wrote to Susan B. Anthony, leader of the National American Woman Suffrage Association, to ask for her help, but died soon thereafter. As she said in 1898: “I went to Philadelphia, studied medicine hard, procured my degree, and have come back to Atlanta, where I have lived all my life, to practice my profession... Some of the best white doctors in the city have welcomed me, and say that they will give me an even chance in the profession. That is all I ask.” The North American Medical Review reported: “She will hang out her shingle for general practice, and says she will make no discrimination on account of color.” Dr. Eliza Grier realized a remarkable achievement.
-
Copy Link
Copied
Setting Their Sights
Confronting Glass Ceilings
By the early 1900s, women had made impressive inroads into the medical profession as physicians, but few had been encouraged to pursue careers as medical researchers. To succeed as scientists, despite opposition from male colleagues at leading institutions, women physicians persisted in gaining access to mentors, laboratory facilities, and research grants to build their careers.
The achievements of these innovators often went unrewarded or unacknowledged for years. Yet these resourceful researchers carved paths for other women to follow and eventually gained recognition for their contributions to medical science.

Close Menu ITEM 0 of 0
Dr. Florence Rena Sabin
Florence Rena Sabin was one of the first women physicians to build a career as a research scientist. She was the first woman on the faculty at Johns Hopkins University School of Medicine, building an impressive reputation for her work in embryology and histolology (the study of tissues). She also overturned the traditional explanation of the development of the lymphatic system by proving that it developed from the veins in the embryo and grew out into tissues, and not the other way around.
Sophia Smith Collection, Smith College
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
-

Microscope like the ones Florence Sabin used, 1917
The Alan Mason Chesney Medical Archives of the Johns Hopkins Medical Institutions-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
-

Looking for Answers
Dr. Florence Sabin examined chick embryos at various stages of growth. She was the first to explain exactly how embryonic cells evolve into blood vessels, blood serum, and red blood cells.
National Museum of Health and Medicine
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
Dr. Sabin's Microscope

Close Menu ITEM 2 of 0
Dr. May Edward Chinn
In 1926, May Edward Chinn became the first African American woman to graduate from the University and Bellevue Hospital Medical College. She practiced medicine in Harlem for fifty years. A tireless advocate for poor patients with advanced, often previously untreated diseases, she became a staunch supporter of new methods to detect cancer in its earliest stages.
George B. Davis, Ph.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 3 of 0
Dr. Gerty Theresa Radnitz Cori
Gerty Theresa Radnitz Cori and her husband, Dr. Carl Cori, were the first married couple to receive a Nobel Prize in science. Gerty Cori was only the third woman ever to win a Nobel Prize, and was the first woman in America to do so.
Becker Medical Library, Washington University School of Medicine
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 4 of 0
Dr. Gerty Theresa Radnitz Cori
Dr. Gerty Theresa Radnitz Cori became the first women in America to win a Nobel Prize in Physiology or Medicine.
Click on the video play button to watch a video on Dr. Cori.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Gerty Radnitz Cori was the first American woman to receive the Nobel Prize in Medicine. She and her husband, Dr. Carl Cori, shared the prize for their discovery of the cycle of carbohydrates in the human body. They had been classmates at the German University of Prague, where Gerty Cori was one of only a few women students. She received her M.D. in 1920. The couple married and began to work in clinics in Vienna. In 1922, concerned that war would break out in Europe for a second time, they immigrated to Buffalo, New York. Carl Cori accepted a position at the State Institute for the Study of Malignant Diseases. Gerty Cori joined him six months later, after securing a job as an Assistant Pathologist. Although the couple was frequently discouraged from working together, they had a dynamic research partnership that proved immensely profitable in their work. Specializing in biochemistry, the husband and wife team began to study how glucose is metabolized in the human body. In 1929, they developed their theory of “the cycle of carbohydrates,” now known as the Cori Cycle. The theory explains how carbohydrates supply energy to muscles during exercise, and then are regenerated and stored until needed again by the muscles. It was the first time the cycle of carbohydrates in the human body had been fully explained and understood, and proved especially useful for the treatment of diabetes. Despite their collaborative partnership in defining the cycle, Carl Cori initially received more professional recognition than Gerty Cori. He was encouraged to abandon the team approach and work alone. He was even offered a job only on the provision that he stop working with his wife. The Cori’s continued in their successful collaboration, however, and in 1931 moved to St. Louis. Carl Cori took up the post of Chair of the Pharmacology Department at Washington University School of Medicine. Over the next sixteen years, Gerty Cori worked alongside him as a research assistant. Together, they made further discoveries that clarified the processes of carbohydrate metabolism, that they had originally laid out in the description of the Cori Cycle. In the mid-1940s, Carl and Gerty Cori received great recognition for their work. Carl Cori was appointed Chair of the new Biochemistry Department in 1946, and Gerty Cori was appointed to a full professorship. The following year, they were awarded the Nobel Prize for the Cori Cycle. They were the first married couple ever to win the Nobel Prize in Medicine.
-
Copy Link
Copied

Close Menu ITEM 5 of 0
Dr. Louise Pearce
Louise Pearce, M.D., a physician and pathologist, was one of the foremost women scientists of the early 20th century. Her research with pathologist Wade Hampton Brown led to a cure for trypanosomiasis (African Sleeping sickness) in 1919.
Courtesy of the Rockefeller University Archives
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 6 of 0
Dr. Louise Pearce
Dr. Louise Pearce’s research helped lead to a cure for trypanosomiasis (African sleeping sickness) in 1919.
Click on the video play button to watch a video on Dr. Pearce.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Louise Pearce volunteered to go alone to the Belgian Congo in 1920 to test a new drug she hoped would cure African sleeping sickness, a disease that was often fatal. She received her M.D. from The Johns Hopkins University in 1912. Looking for work, she wrote to Dr. Simon Flexner, Director of the Rockefeller Institute in New York City, requesting a research position. Dr. Flexner supported her application, and Dr. Louise Pearce became the first woman to work directly with him. In 1910, an arsenic-based drug called Salvarsan was found to be an effective treatment for syphilis. Scientists had hopes of developing other arsenic-based drugs. Dr. Flexner asked his research team to try and find an arsenical compound for use against African sleeping sickness. They succeeded. Tryparsamide, they found, destroyed the infectious agent of sleeping sickness in animals. In 1919, these results were announced in the Journal of Experimental Medicine. A severe outbreak of African sleeping sickness broke out in the Belgian Congo in 1920. While in Africa, Dr. Pearce administered and studied the effects of the tryparsamide on seventy patients. The results were spectacular: the parasites were driven from circulating blood within days and totally eradicated within weeks. Symptoms cleared up and general health was restored in a large proportion of even the most severe cases. Belgian officials were impressed by the results. Dr. Pearce was awarded the Ancient Order of the Crown and elected a member of the Belgian Society of Tropical Medicine. Three decades later, in 1953, she was invited to Brussels to receive the King Leopold III Prize and an award of ten thousand dollars. After her success in the Belgian Congo, Dr. Pearce returned to the Rockefeller Institute, and was promoted to Associate Member in 1923. Teamed with Dr. Wade Hampton Brown, she studied susceptibility and resistance to infection. They discovered they could transplant certain cancers from one rabbit to another. The Brown-Pearce tumor was the first known transplantable tumor, aiding research into malignant tumors in cancer laboratories around the world. By 1940, more than two dozen hereditary diseases and deformities were studied in the tumors of the research team’s rabbits. After the death of Wade Hampton Brown in 1942, Dr. Pearce focused on writing up their research findings, until her retirement in 1951. After a short illness, she died at her home in New Jersey in 1959.
-
Copy Link
Copied

Close Menu ITEM 7 of 0
Dr. Anna Wessels Williams
Anna Wessels Williams, M.D., worked at the first municipal diagnostic laboratory in the United States, at the New York City Department of Health. She isolated a strain of diphtheria that was instrumental in the development of an antitoxin for the disease. She was a firm believer in the collaborative nature of laboratory science, and helped build some of the more successful teams of bacteriologists, which included many women, working in the country at the time.
The Schlesinger Library, Radcliffe Institute, Harvard University
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 8 of 0
Dr. Anna Wessels Williams
Dr. Anna Wessels Williams isolated a strain of bacteria that scientists used to develop the treatment for diphtheria.
Click on the video play button to watch a video on Dr. Wessels Williams.
-
ReadBiography
-
MedlinePlus
-
Transcript
In the 1800s, diphtheria was a deadly infectious disease without cure. Dr. Anna Wessels Williams isolated a strain of the diphtheria bacillus crucial to the development of an antitoxin that helped eradicatethe disease in New York City. Dr. Williams worked at the New York City Department of Health, in the first municipal diagnostic laboratory in America. She researched the spread of infectious diseases like diphtheria and polio, then sought ways to protect people and lower the rates of infection. Dr. William H. Park was the director of the lab, and the two collaborated. Together, they worked on developing an antitoxin for diphtheria. In her first year of work, Dr. Williams isolated the strain and by the fall of that year, physicians across Manhattan issued the diphtheria antitoxin free of charge, helping to eradicate the disease among the city’s poor. Dr. Williams was appointed to a full-time staff position as assistant bacteriologist. She shared credit with William H. Park for the discovery, which became known as the Park-Williams Strain. She recognized the collaborative nature of laboratory research, and later said she was “happy to have the honor of having my name thus associated with Dr. Park.” In 1896, Dr. Williams traveled to the Pasteur Institute in Paris hoping to develop an antitoxin for scarlet fever. The research going on in Paris inspired her, and she became interested in rabies. Returning to the U.S., she brought back a culture of the rabies virus and worked to develop a better way to diagnose it. Her method surpassed the original test, and became the model technique for the next thirty years. She was promoted to Assistant Director of the New York City Department of Health laboratory in 1905 and continued to work alongside Dr. Park. Together they wrote a textbook on micro-organisms for students, physicians, and health officers that quickly became a classic text. In 1929, they published “Who’s Who Among the Microbes,” thought to be one of the earliest books on the topic written especially for the public. In 1914, Dr. Williams was elected president of the Women’s Medical Society of New York. In 1931, she was elected to the laboratory section of the American Public Health Association, and the following year became the first woman appointed chair of the section. In addition to her groundbreaking research, she helped build some of the most successful teams of bacteriologists—including many women—working in the country at the time.
-
Copy Link
Copied

Close Menu ITEM 9 of 0
Dr. Jane Cooke Wright
Dr. Jane Wright analyzed a wide range of anti–cancer agents, explored the relationship between patient and tissue culture response, and developed new techniques for administering cancer chemotherapy. By 1967, she was the highest ranking African American woman in a United States medical institution.
National Library of Medicine
-
ReadBiography
-
DigitalCollections
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 10 of 0
Dr. Jane Cooke Wright
Dr. Jane Cook Wright advanced chemotherapy techniques through her pioneering cancer research.
Click on the video play button to watch a video on Dr. Wright.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Jane Wright made her mark in cancer research, developing new techniques for administering chemotherapy and evaluating new treatments for the disease. Jane Wright grew up in a wealthy and prestigious family in New York City. Her father, Dr. Louis Wright, was one of the first black graduates of Harvard University Medical School. In the late 1930s, he founded the Cancer Research Center at Harlem Hospital where Jane Wright would later do some of her most important medical research. Jane Wright grew up during the Harlem Renaissance. African American artists, musicians, writers, and political activists were celebrating their culture, and challenging America’s racial barriers. In a time of great aspirations, Jane Wright was fortunate to have the support and guidance of her family, as well as access to a fine education. Smith College offered her a four-year academic scholarship to study art. In her junior year, at her father’s request, she changed her major to pre-med. She enrolled on a full academic scholarship at New York Medical College where the majority of students were white. Jane Wright was elected president of the Honor Society and vice president of her class. She graduated with honors in 1945. Four years later she joined her father, then the Director of the Cancer Research Foundation at Harlem Hospital. Together, they experimented with different chemical agents on leukemia in mice. While her father worked in the lab, she performed patient trials. In 1949, the Wrights began treating patients with anti-cancer drugs. Several patients experienced some degree of remission. When her father died in 1952, Dr. Jane Wright succeeded him as director. In 1955, she joined the faculty of New York University as an Associate Professor of Surgical Research, and Director of Cancer Research. There, she continued her work with chemotherapy studying a variety of anti-cancer drugs and developing new techniques for delivering potent drugs to tumors deep within the body. She created a database, cross-referencing cancers and patients, to help determine the effectiveness of these drugs. Later, Dr. Wright began experimenting with combinations of anti-cancer drugs. Because she believed most cancers were caused by viruses, she investigated a new class of anti-cancer agents comparable to antibiotics. During her forty-year career, she produced more than seventy-five research papers on cancer chemotherapy, and in 1971, became the first woman elected president of the New York Cancer Society.
-
Copy Link
Copied
Making Their Mark
Bringing fresh perspectives to the profession of medicine, women physicians often focused on issues that had received little attention-the social and economic costs of illness, new research and treatments for women and children, and the low numbers of women and minorities entering medical school and practice.
As the first to address some of these needs, women physicians often led the way in designing new approaches to public health policy, illness, and access to medical care. The revival of the civil rights and women's movements and passage of equal opportunity legislation in the 1960s led to a dramatic increase in the numbers of women and minorities entering medicine.
Making Their Mark
Caring for Communities
Many early advocates of the rightful place of women in the professions argued that women had a special obligation to those most at risk. By the first decades of the 1900s, women physicians were establishing innovative public health programs and labor reforms designed to protect the most vulnerable members of society.
By succeeding in work considered “unsuitable” for women, these leaders overturned prevailing assumptions about the supposedly lesser intellectual abilities of women and the traditional responsibilities of wives and mothers. [or As the century progressed, the discrimination experienced by women and minorities fueled broad social movements for change. Women physicians involved in this struggle became advocates for those suffering from neglect or abuse.]

Close Menu ITEM 0 of 0
Dr. Alice Hamilton
Alice Hamilton was a leading expert in the field of occupational health. She was a pioneer in the field of toxicology, studying occupational illnesses and the dangerous effects of industrial metals and chemical compounds on the human body. She published numerous benchmark studies that helped raise awareness of dangers in the workplace. In 1919, she became the first woman appointed to the faculty at Harvard Medical School, serving in their new Department of Industrial Medicine. She also worked with the state of Illinois, the U.S. Department of Commerce, and the League of Nations on various public health issues.
Alice Hamilton, M.D., National Library of Medicine, Images from the History of Medicine, B014009
-
ReadBiography
-
DigitalCollections
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Martha May Eliot
Dr. Martha May Eliot worked for the Children’s Bureau, a national agency established in 1912 to improve the health and welfare of American children, for over 25 years. First employed as director of the bureau’s Division of Child and Maternal Health, Eliot went on to become assistant chief, and then chief, of the whole organization. She was the only woman to sign the founding document of the World Health Organization, and an influential force in children’s health programs worldwide.
Martha May Eliot, M.D., National Library of Medicine, Images from the History of Medicine, B09844, photograph by Bachrach
-
ReadBiography
-
DigitalCollections
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Healthy femur (left) and femur showing the effects of rickets (right)
Children’s bones contain growth plates—areas of soft cartilage that lengthen before being replaced by hard bone. With rickets, the bone's growth plate widens as soft cartilage cells accumulate.
The bones of a child with rickets (right) are too soft and bend under the pressure of body weight. Proper diet and adequate sunlight provide the vitamin D necessary to build strong bones (left). Dr. Martha May Eliot’s work provided insight on how to treat this disease.
National Museum of Health and Medicine, Armed Forces Institute of Pathology
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 3 of 0
Dr. Helen Rodriguez-Trias
Through her efforts to support abortion rights, abolish enforced sterilization, and provide neonatal care to underserved people, Helen Rodriguez–Trias expanded the range of public health services for women and children in minority and low–income populations in the United States, Central and South America, Africa, Asia, and the Middle East.
Helen Rodriguez–Trias, M.D., JoEllen Brainin–Rodriguez M.D., photograph by Rafael Pesquera
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 4 of 0
Dr. Helen Rodriguez-Trias
Dr. Helen Rodriguez–Trias worked to improve access to health services for women and children in underserved communities, advocated for women’s rights, and served as the first Latina president of the American Public Health Association.
Click on the video play button to watch a video on Dr. Rodriguez–Trias.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Helen Rodriguez-Trias wanted to study medicine because it combined the things she loved the most—science and people. She graduated from the University of Puerto Rico in 1959 and moved to New York, where she married and had three children. After seven years, she returned to the University of Puerto Rico to study medicine. She saw it as a direct way to contribute to society—by helping individuals instead of working through groups or organizations. She received an M.D. with the highest honors in 1960. During her residency, Dr. Rodriguez-Trias established the first center in Puerto Rico for the care of newborn babies. Under her direction, the hospital’s death rate for newborns decreased 50 percent within three years. In 1970, she returned to New York City to serve the Puerto Rican community in the South Bronx. Working at Lincoln Hospital, she led community campaigns against lead paint, unprotected windows and other health hazards. She also taught at City College, raising students’ awareness of the real conditions in the neighborhoods they served. Dr. Rodriguez-Trias saw the critical links between public health and social and political rights, and expanded her work to a broader international community. She said, “I think my sense of what was happening to people’s health... was that it was really determined by what was happening in society— by the degree of poverty and inequality you had.” Working as an advocate for women’s reproductive rights, she campaigned for change at a policy level. She worked especially for low-income populations in the United States, Central and South America, Africa, Asia, and the Middle East. She fought for reproductive rights, worked with women with HIV, and joined the effort to stop sterilization abuse. Government-sponsored sterilization programs led to hundreds of unwanted sterilizations. (Dr. Helen Rodriguez-Trias) “Sterilization has been pushed really internationally as a way of population control. And there is a difference between population control and birth control. Birth control exists as an individual right. It’s something that should be built into health programming. It should be part and parcel of choices that people have. And when birth control is really carried out, people are given information, and the facility to use different kinds of modalities of birth control. While population control is really a social policy that’s instituted with the thought in mind that there’s some people who should not have children or should have very few children, if any at all. I was working in Puerto Rico in the medical school in those years, the decade of 1960 to 1970. And one of the things that seemed pretty obvious to us then was that Puerto Rico was being used as a laboratory. And it was being used as a laboratory for the development of birth control technology.” In 1979, Dr. Rodriguez-Trias testified before the Department of Health, Education and Welfare for the passage of federal sterilization guidelines, which she helped to draft. These require a woman’s consent to sterilization, offered in a language she can understand, and set a waiting period between the consent and the operation. Toward the end of her life, she said, “I hope I’ll see in my lifetime a growing realization that we are one world. And that no one is going to have quality of life unless we support everyone’s quality of life. Not on a basis of do-goodism, but because of a real commitment. It’s our collective and personal health that’s at stake.” In 2001, President Clinton presented her with a Presidential Citizen’s Medal for her work on behalf of women, children, people with HIV and AIDS, and the poor. Later that year, Helen Rodriguez-Trias died of complications from cancer.
-
Copy Link
Copied

Close Menu ITEM 5 of 0
Dr. Mary Steichen Calderone
Dr. Mary Steichen Calderone brought an uncomfortable subject to the forefront of public debate in her work in sex education. Beginning in the 1950s, when public discussion of such issues was considered highly controversial, Dr. Calderone flouted convention by speaking out in the first place, and as a woman broaching such a topic. In 1964, she founded the Sex Information and Education Council of the United States (SIECUS), to promote sex education for children and young adults.
The Schlesinger Library, Radcliffe Institute, Harvard University
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 6 of 0
Dr. Mary Steichen Calderone
Dr. Mary Steichen Calderone advocated for sex education, founding the Sex Information and Education Council of the United States (SIECUS).
Click on the video play button to watch a video on Dr. Calderone.
-
ReadBiography
-
MedlinePlus
-
Transcript
(Dr. Mary Steichen Calderone) “What is this film really saying? First of all, that sex is normally and properly a part of each one of us, from babyhood on. Secondly, that understanding and acceptance of the normal sexuality of children of all ages is a must for every adult. What children need from us is information to answer all of their questions. This is a must. Just to protect them against the misinformation and wrong attitudes that are all around us.” In the 1950s, an era when talking publicly about sex was taboo, Dr. Mary Steichen Calderone spoke out about sexuality as an inherent part of being human. As Medical Director of Planned Parenthood, she began to change the way that Americans talked about sex. Because of the climate of the time, her ideas were controversial, especially so because a woman was not supposed to mention such things. But her advice was common sense, applicable to both sexes, and she delivered it with medical acumen, ease, and candor. As a physician, she brought a medical perspective to the subject to explain human sexuality as a natural part of life. Planned Parenthood provided contraception and sexual health information and resources for the public. Dr. Calderone also addressed the concept of separating sex from reproduction. She promoted sex as a healthy, normal part of life, worthy of public discussion. In 1964, Dr. Calderone left Planned Parenthood to create The Sex Information and Education Council of the United States. The Council provided information for schools and for young people. Through her own books, Dr. Calderone advised parents on positive ways to talk to their children about sex. Her efforts helped young people gain the confidence and knowledge to enjoy safe and healthy sex lives in adulthood. Mary Steichen Calderone won many awards, including, the Woman of Conscience Award in 1968, and the Elizabeth Blackwell Award for Distinguished Service to Humanity. In 1971, the Ladies Home Journal named her one of “America’s 75 Most Important Women.” Four years later, she was listed among the “50 Most Influential Women in the U.S.” The atmosphere that is so vital today, that allows for informed discussions about reproductive health, unwanted pregnancy, HIV, AIDS and other sexually transmitted diseases, follows from initiatives begun in the 1950s by Dr. Mary Steichen Calderone. (Dr. Mary Steichen Calderone) “Most of all, children need parents who can show love—for each other, and for their children. For in such a home, sharing knowledge of this great and universal human experience can only serve to strengthen family ties.”
-
Copy Link
Copied

Close Menu ITEM 7 of 0
Dr. Dorothy Celeste Boulding Ferebee
Dr. Dorothy Ferebee was a tireless advocate for racial equality and women’s health care. In 1925, in a derelict section of Capitol Hill, she established Southeast Neighborhood House, to provide health care for impoverished African Americans. She also set up the Southeast Neighborhood Society, with playground and day care for children of working mothers. At Howard University Medical School, she was appointed director of Health Services. She was founding president of the Women’s Institute an organization that serves educational, community, government, and non–profit organizations, as well as individual patients.
Ferebee/Edwards Papers, Moorland–Spingarn Research Center, Howard University
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 8 of 0
Dr. Dorothy Celeste Boulding Ferebee
Dr. Dorothy Boulding Ferebee advocated for civil rights, women’s health care, and public health, and worked to expand access to health care in poor African American communities.
Click on the video play button to watch a video on Dr. Ferebee.
-
ReadBiography
-
MedlinePlus
-
Transcript
“As a young girl, I would nurse and help the birds that fell out of trees,” recalled Dr. Dorothy Boulding Ferebee. While her friends played with toys, she healed injured animals. At an early age, she knew she wanted to become a doctor. After graduating fifth in her class from Tufts University School of Medicine in 1924, Dorothy Boulding, like other qualified African American physicians across the country, was denied internships at white hospitals. Determined to find equal opportunity to complete her training, Dr. Boulding took an internship at Freedman’s Hospital in the Capitol Hill neighborhood of Washington, D.C. One of the few hospitals administered by African Americans, it provided health care to the city’s black community. In 1925, after completing her internship, Dr. Boulding opened her own practice in the Capitol Hill neighborhood. The community was very poorand did not have an ambulance service. Dr. Boulding was determined to bring basic care to those who could not afford it. (Dr. Dorothy Ferebee) “So I learned a great deal about the needs of the negro people in Washington, because most of them were concentrated in Southeast. So it was there that I learned there was very little opportunity for the children. Even though they were in school, they weren’t learning anything. And then it occurred to me, there’s something wrong with this town. Anytime a child goes hungry, and the mother has to work and leave her child home like this we need some place for children. We need a day care center.” Concerned about the needs of families in the community, she set up the Southeast Neighborhood Society, with playgrounds and day care for children of working mothers. In 1925, Dr. Boulding joined the faculty of Howard University Medical School, where she met, and later married Claude Thurston Ferebee, a dentist and university instructor. In 1934, she was appointed Medical Director of the Mississippi Health Project. (Dr. Dorothy Ferebee) “Going to Mississippi was quite an ordeal. In all of those counties, the influential people were the plantation owners. They’re the ones that decided what could be done,what could not be done. So, reluctantly they allowed us to start a clinic. But they would not allow the blacks on the plantation to leave their job of picking cotton and hoeing the weeds—would not allow them to come to any of the five clinics that we had proposed. So here we were, in Mississippi with all the materials that we had bought, the drugs that we had bought, all of the things necessary for the health of young children, and couldn’t use them because these plantation owners would not allow the negroes to come to us. So we had a little consultation, and we said, ‘Well, if they can’t come to us, we’ll go them.’ So it was an educational teaching job as well as a health job.” Despite threats by hostile whites, project workers launched vaccine programs against smallpox and diphtheria throughout poor communities. They also treated venereal disease and widespread malnutrition. Members of the Alpha Kappa Alpha Sorority financed, designed, and implemented the Project for two to six weeks every summer from 1935 to 1942. In 1949, Dr. Ferebee was appointed Director of Health Services for the Howard University Medical School. When she was in her sixties, President John F. Kennedy appointed her to the Council for Food for Peace, and she toured Africa for five months, lecturing on preventive medicine. Doctor Dorothy Boulding Ferebee died in 1980, at the age of ninety.
-
Copy Link
Copied

Close Menu ITEM 9 of 0
Dr. Fernande Marie Pelletier
Sister Fernande Pelletier, M.D., a member of the Medical Mission Sisters (founded 1925), has worked overseas for more than forty years, carrying out the mission of her order in Ghana and offering medical care to underserved populations. Her incredible devotion and service has been rewarded by the Ghanaian government, and in rural communities far from fully–equipped hospitals, she continues to care for those in need.
Medical Mission Sisters
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 10 of 0
Dr. Fernande Marie Pelletier
Dr. Fernande Pelletier works as a Medical Mission Sister to deliver health care to underserved communities in Ghana.
Click on the video play button to watch a video on Dr. Pelletier.
-
ReadBiography
-
Transcript
Dr. Fernande Pelletier went to Africa in 1961 as a Medical Mission Sister. A graduate of the Georgetown University Medical School, she was thirty years old when she left home to begin her service. Her destination was the city of Berekum, Ghana, where she has now lived and served for over forty years. Throughout her service, Dr. Pelletier has had to overcome language, technological, and cultural barriers. She learned the local dialect, Twi, so she could talk directly with her patients, and the midwives and nurses she has trained over the years. She immerses herself in the local culture, trying to understand the ways that her patients think about their illnesses. Her dedication to her work has been celebrated by the Ghanian Government, who awarded Dr. Pelletier the Grand Medal for outstanding rural medical work. In addition to medical supplies, Dr. Fernande Pelletier provides AIDS education, home visits to new mothers, and training for new medical health workers. Using the Holy Family Hospital Outreach Vehicle for travel, she reaches remote areas without hospitals and doctors, caring for her patients’ needs in any way she can. Dr. Pelletier respects the spiritual beliefs of her patients and concentrates on relieving their illnesses or injuries. She explains, “By our action, we express our religious belief. Not ’I heal you and now you join my religion’... But by action; by healing people out of love and making them whole. That, I think, speaks louder.” Dr. Pelletier continues to serve the goals of the Medical Mission Sisters, making good health care accessible to poor patients in remote areas.
-
Copy Link
Copied

Close Menu ITEM 11 of 0
Dr. M. Joycelyn Elders
Joycelyn Elders, the first person in the state of Arkansas to become board certified in pediatric endocrinology, was the sixteenth Surgeon General of the United States, the first African American and only the second woman to head the U.S. Public Health Service. Long an outspoken advocate of public health, Elders was appointed Surgeon General by President Clinton in 1993.
Parklawn Health Library
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 12 of 0
Dr. M. Joycelyn Elders
Dr. Joycelyn Elders is the first African American and second woman to serve as the U.S. surgeon general.
Click on the video play button to watch a video on Dr. Elders.
-
ReadBiography
-
MedlinePlus
-
Transcript
Joycelyn Elders was born a tenant farmer’s daughter in rural Arkansas. At age five, she worked in the cotton fields while attending a segregated school thirteen miles from home. During harvest time, from September to December, she often missed school. She did well enough, though, to earn a scholarship to the all-black, liberal arts Philander Smith College in Little Rock. Making it through college was a family affair. Joycelyn Elders cleaned floors, while her brothers and sisters did extra work in the fields and chores for neighbors to help earn her bus fare. In college, she worked hard and especially enjoyed biology and chemistry. She hoped to become a lab technician. Her ambitions dramatically changed when she heard a talk by Dr. Edith Irby Jones, the first African American to attend the University of Arkansas Medical School. Though Elders had never even met a doctor until she was sixteen years old, she decided it was possible to become a physician, like Dr. Jones. In 1956, like her role model, she enrolled at the University of Arkansas Medical School. Two years before, the Supreme Court had declared “separate but equal” education unconstitutional. Despite that ruling, Elders was prohibited from sharing dining facilities with the other students on campus. In spite of the inauspicious circumstances early in her life, Dr. Elders was appointed Surgeon General of the United States by President Bill Clinton in 1993. In this prominent post, Dr. Elders continued to promote the issues she had been committed to in her previous work as head of the Arkansas Department of Health, where she had been especially concerned with the health of young people and campaigned for the introduction of a range of innovative educational programs to the school curriculum. Within five years, she nearly doubled childhood immunizations in Arkansas, expanded the state’s pre-natal care program, and increased home-care options for the chronically and terminally ill. As Surgeon General, Dr. Elders concluded it was her responsibility to get people to listen and talk about difficult subjects, since only then can change come about. She again concentrated on the health of young people and led the national debate on the prevention of substance abuse, and sex education for teenagers. Some considered her focus on these issues controversial, and she left office after 15 months. She returned to the University of Arkansas as a faculty researcher and was appointed professor at the Arkansas Children’s Hospital. Now retired from practice, Dr. Elders is a professor emeritus at the University of Arkansas School of Medicine and remains active in public health education.
-
Copy Link
Copied
Making Their Mark
Making Discoveries
Women physicians, who have often been discouraged from pursuing the most prestigious specialties, nevertheless have seized opportunities in medical research and practice. In some instances, they have brought new expertise to neglected areas of research. In others, they have carved out new roles for their interests within existing specialties.
The breakthrough discoveries in medical research of women physicians benefit all of us, patients and practitioners.

Close Menu ITEM 0 of 0
Dr. Virginia Apgar
Virginia Apgar, M.D., the first woman to become a full professor at Columbia University College of Physicians and Surgeons, designed the first standardized method for evaluating the newborn’s transition to life outside the womb–the Apgar Score.
The Mount Holyoke College Archives and Special Collections
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Helen Brooke Taussig
Helen Brooke Taussig is known as the founder of pediatric cardiology for her innovative work on “blue baby” syndrome. In 1944, Taussig, surgeon Alfred Blalock, and surgical technician Vivien Thomas developed an operation to correct the congenital heart defect that causes the syndrome. Since then, their operation has prolonged thousands of lives, and is considered a key step in the development of adult open heart surgery the following decade. Dr. Taussig also helped to avert a thalidomide birth defect crisis in the United States, testifying to the Food and Drug Administration on the terrible effects the drug had caused in Europe.
The Alan Mason Chesney Medical Archives of The Johns Hopkins Medical Institutions
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Dr. M. Irené Ferrer
As a young physician, Dr. Irené Ferrer was the first woman to serve as chief resident at Bellevue Hospital, where she was given a prestigious opportunity: to work with a leading team of cardiologists who were developing the cardiac catheter. Dr. Ferrer played a vital role in the Nobel prize–winning project, which was also an important step in the development of open–heart surgery.
Marianne Legato, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 3 of 0
Dr. M. Irené Ferrer
Dr. Irené Ferrer helped develop the cardiac catheter and was the first woman chief resident at Bellevue Hospital, Columbia University.
Click on the video play button to watch a video on Dr. Ferrer.
-
ReadBiography
-
MedlinePlus
-
Transcript
As a young physician, Dr. Irené Ferrer was the first woman to serve as chief resident at Bellevue Hospital, where she was given a prestigious opportunity: to work with a leading team of cardiologists who were developing the cardiac catheter. Had it not been for the lack of male candidates during World War II, it is unlikely that a woman physician would have been given such a chance. But Dr. Ferrer played a vital role in the project. The catheter was an important step toward open-heart surgery and earned the team a Nobel Prize in 1956. Dr. Ferrer also collaborated with IBM to make computerized interpretation of electrocardiograms possible for the first time. From 1953 to 1986, she was director of the Electrocardiographics Department at Doctors Hospital. Since 1986, she has served as an honorary consultant at Presbyterian and St. Luke’s-Roosevelt and is professor emeritus at Columbia University. Special among her many honors, is the M. Irené Ferrer Professorship in Women’s Health and Gender-specific Medicine at Columbia University, established in her name by the Partnership for Women’s Health founded and directed by Dr. Marianne Legato. Dr. Marianne Legato was one of the many younger physicians Dr. Irené Ferrer mentored in an extraordinary way throughout her career. When Marianne Legato left medical school because she could not afford the tuition, Dr. Ferrer convinced the Dean to let Legato return and paid for the rest of her education. (Dr. Marianne Legato): “And Dr. Ferrer herself went back and personally called on the Dean of NYU and said, ‘I’m gonna pay for this, young woman’s education. I will guarantee a good performance, and I want you to take her back’, which he did. After that I became really a member of the Ferrer family, and they were a wonderful, wonderful force in my own life and in my own development. It was a wonderful family to which I had sort of been added, and they really made my career possible.” Dr. Ferrer’s contribution to the development of the cardiac catheter and the compelling example she gave to medical students was based on her extraordinary relationship with her patients. (Dr. Marianne Legato): “She became devoted to many of her patients, whom she dearly loved. Her love of patients was really remarkable and one of the things about her that made her so engaging as a role model for us. So that combination of intellectual brilliance and real love of the patient was sort of a winning combination for those of us who were lucky enough to be her students.”
-
Copy Link
Copied

Close Menu ITEM 4 of 0
Dr. Marilyn Hughes Gaston
Marilyn Hughes Gaston, M.D., faced poverty and prejudice as a young student, but was determined to become a physician. She has dedicated her career to medical care for poor and minority families, and campaigns for health care equality for all Americans. Her 1986 study of sickle–cell disease led to a nationwide screening program to test newborns for immediate treatment, and she was the first African American woman to direct a public health service bureau (the Bureau of Primary Health Care in the United States Department of Health and Human Services).
Parklawn Health Library
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 5 of 0
Dr. Marilyn Hughes Gaston
Dr. Marilyn Hughes Gaston did important research into sickle–cell disease and became the first African American woman to direct a bureau of the U.S. Public Health Service.
Click on the video play button to watch an interview with Dr. Gaston.
-
ReadBiography
-
MedlinePlus
-
Transcript
One day I was in the living room with my mother. I grew up in the projects, which is what used to be called low-income housing for poor people. And we only had three small rooms, and that day she fainted in the living room. And I had no idea what was wrong. It was very frightening to me, and back then we didn’t have 911 and so I didn’t really know what to do. But the long and short of this is that she had cancer of the cervix. We were poor, we were uninsured, she was not getting health care. And from that point on, I knew that I wanted to do something to change that situation. At that time there were not many women in medicine. There certainly weren’t many African Americans. So I had no role models, and I had no encouragement to go into medicine. My counselors all said, oh, no, don’t worry about that. You’ll never get admitted as a woman. You’ll never get admitted as an African American, or as an African American woman, and besides, you’re too poor to go. You know, you’ll never have the money. But the motivation—I knew I really wanted to do this. And I had wonderful mentors that said, don’t let your dreams go. And I guess in all fairness, back then, it did seem like an impossible dream at the time. So that these issues were very clear early on to me, and they have remained prominent in my career. And I have spent a career trying to change this, and trying to get health care to disadvantaged, underserved people throughout the nation. I spent some time at the National Institutes of Health. And one of the projects that I did while I was there was working with sickle cell disease, especially looking at the problem that babies with sickle cell disease die very suddenly—especially they’re at risk in the first three years of life. I led a study where we looked at can’t we prevent this? If by giving babies penicillin prophylactically, before they get the fever, before they get the infection—can’t we save some lives? This study was so successful we stopped it midway—because the results were so compelling. The babies that got the penicillin prophylactically definitely did not have the infections, and it was a study that saved lives. And it is saving lives now. Worldwide. You know, because sickle cell disease is a worldwide problem. I always tell students that your heroes and your sheroes are not just in the history books, they’re not just on TV, but they’re all around you. And to look for them, and to ask them to mentor you. Don’t just passively and say, oh, I wish I could have that person, ask them. And I always remind them, you know, that they’ll always say yes. Because we’re always so flattered, and we say, oh, yes. I would be glad to be your mentor.
-
Copy Link
Copied

Close Menu ITEM 6 of 0
Dr. Janet Davison Rowley
In the early 1970s, Dr. Janet Rowley identified a process of “translocation,” or the exchange of genetic material between chromosomes in patients with leukemia. This discovery, along with Dr. Rowley’s subsequent work on chromosomal abnormalities, has revolutionized the medical understanding of the role of genetic exchange and damage in causing disease.
David Bentley Photography, Inc.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 7 of 0
Dr. Janet Davison Rowley
Dr. Janet Davison Rowley identified the translocation of chromosomes as the cause of leukemia and other cancers.
Click on the video play button to watch a video on Dr. Rowley.
-
ReadBiography
-
MedlinePlus
-
Transcript
In the 1970s, Dr. Janet Rowley brought a new understanding to the role of genetics in disease when she demonstrated that the translocation of chromosomes played a significant role in some cancers. A dedicated student, she received a scholarship to the University of Chicago when she was fifteen years old, and completed the last two years of high school and the first two years of college in an accelerated program of study at the University. She stayed on to complete her pre-medical training and attend the medical school and graduated with an M.D. degree in 1948. She married Donald Rowley, also a physician, the day after graduating from medical school. For twenty years, Dr. Rowley chose to work part-time, in order to be with her children. When the youngest was twelve, she turned to full-time research. She became interested in genetics while working at the Dr. Julian Levison Foundation, a clinic for children with developmental disabilities. In 1961, funded by the National Institutes of Health, she traveled to Oxford, England, to study chromosomes at a radiobiology laboratory. There, she investigated the pattern of DNA replication in normal and abnormal human chromosomes. A year later, at the end of the project, Dr. Rowley returned to the University of Chicago to continue her research. In the early 1970s, she brought a new perspective to the understanding of cancer by demonstrating that the abnormal chromosome implicated in certain types of leukemia was also involved in a translocation, in some cases. By 1990, over seventy chromosomal translocations had been identified across different types of cancer. Today, Dr. Rowley continues her research at the University of Chicago. She holds the position of the Blum-Riese Distinguished Service Professor, and serves as the Interim Deputy Dean for Science. In 1998, Dr. Janet Rowley was awarded the prestigious Lasker Award for her work on translocation and cancer.
-
Copy Link
Copied

Close Menu ITEM 8 of 0
Dr. Katherine M. Detre
Dr. Katherine M. Detre has been named a distinguished professor of epidemiology at the University of Pittsburgh’s Graduate School of Public Health, in recognition of her many achievements. A leading expert in epidemiological analysis, she has designed and led large-scale health studies undertaken across the country.
Katherine Maria Drechsler Detre, M.D., M.P.H., Dr.P.H.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 9 of 0
Dr. Katherine M. Detre
Dr. Katherine M. Detre was a leading epidemiologist, spearheading large–scale health studies.
Click on the video play button to watch a video on Dr. Detre.
-
ReadBiography
-
Transcript
Dr. Katherine Detre is a research leader in large-scale studies investigating disease and risk factors across populations. She grew up in Budapest, Hungary during the Nazi occupation in World War II. To cope with the loss of some of her closest family members, she devoted herself to her studies. In Budapest, she trained at Pazmany Peter Medical School. In 1949, she received an International Student Service Award to study in Canada. Three years later, she received her medical degree from Queen’s University Medical School in Ontario, and followed that with a Residency in Internal Medicine at Queen Mary Veterans Hospital. Shortly after, she came to the United States and married Dr. Thomas Detre. In 1956, she moved to Yale University where she specialized in Biometry, the application of statistics to the biological sciences. In 1960, Dr. Katherine Detre traveled to Hiroshima, Japan to study heart disease. Returning to Yale, she earned a Master of Public Health Degree in 1964, and a doctorate in 1967. Today, Dr. Detre serves as a Professor of Epidemiology at the University of Pittsburgh. In 2000, she was awarded a major grant for an expansive study of coronary artery disease and diabetes. The research spans forty areas nationwide, and includes three thousand patients. Recently, she received the highest honor awarded by the University; that of “Distinguished Professor.” The prestigious title honors her “extraordinary, internationally-recognized, scholarly achievement.”
-
Copy Link
Copied

Close Menu ITEM 10 of 0
Dr. Ruth E. Dayhoff
Ruth E. Dayhoff is at the forefront of medical informatics. As the medical technologies used to diagnose disease have become more complex, corresponding new information systems have been developed to analyze, store, and present the new types of data. Dr. Dayhoff followed her mother, Dr. Margaret Oakley Dayhoff, into the field she pioneered in the 1960s, heading the VistA Imaging Project at the Department of Veterans Affairs—a unique, innovative system that will eventually be implemented in all VA medical centers across the United States.
Ruth E. Dayhoff, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 11 of 0
Dr. Ruth E. Dayhoff
Dr. Ruth E. Dayhoff is a leader in the field of medical informatics, heading the VistA Imaging Project at the Department of Veteran Affairs.
Click on the video play button to watch an interview with Dr. Dayhoff.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Ruth E. Dayhoff I had been interested for a long time in the use of computers in medicine. I felt that by bringing a technology into medicine that could be used by many, many doctors, I could make a bigger difference than I would as a single practicing physician. It was difficult because I had to actually persuade people that computers were important, and that they needed a physician to help them with medical computing—that I wasn’t just a programmer. I also had a job working on medical databases, the sorts of databases that would hold patients’ information. And I began to think that wouldn’t it be wonderful if we could combine both the database technology and the image technology into one system, so that you wouldn’t have to store your images on tapes with labels, or on disks, that you couldn’t find what you needed, that it would be linked together. You’d just check the database and it would show you the image. So this idea further developed when I visited the VA (Veterans Affairs) Medical Center and the doctors looked at the system and said, “Wow, this would really help us in the hospital.” So that was the beginning of the VISTA Imaging Project. The VISTA Imaging System is an integrated computer system that combines images with patient records in an online system. The software runs on workstations throughout the medical center, providing physicians with the information that they need to treat their patients. And it’s actually running in over a hundred hospitals across the country today. They started using the system on the wards. When they were treating a patient they found that by looking at an image, they had a sense of the urgency. For instance, if they saw a vessel in the heart that was 90 percent occluded, 90 percent didn’t tell them very much. But when they saw the image they could realize the impact that the problem was having on the patient. They could even show the image to the patient and explain to them what the problem was, then let the patient be part of the decision making process. So they were really very enthusiastic about it. It was very important to work with people who were taking the system and putting it into their process of practicing medicine, and in some cases changing the process to take advantage of the technology. And that’s really what we want to do, bringing the technology to medicine.
-
Copy Link
Copied
Making Their Mark
Enriching Medical Education
Many patients find that doctors from their own communities are better able to understand their concerns. Because the women physicians who train future physicians recognize the value of diverse perspectives, they are developing innovative teaching strategies and programs to attract students from many backgrounds to all specialties. To help students succeed in medical school, women physicians act as mentors, advisors, and role models.
Women physicians are enlarging the base of students who aspire to careers in medicine, as well as expanding the skills that all medical students take into successful practice.

Close Menu ITEM 0 of 0
Dr. Katherine A. Flores
Katherine A. Flores established two programs to encourage disadvantaged students to pursue careers in medicine: the Sunnyside High School Doctor’s Academy and the middle school Junior Doctor’s Academy. These programs provide academic support and health science enrichment to young people who might not otherwise be successful in their educational experiences—or be thinking about medical careers.
Katherine A. Flores, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Linda Dairiki Shortliffe
Dr. Linda M. Dairiki Shortliffe built a successful career in the relatively new field of pediatric urology when very few women surgeons were doing such work. Since 1988, she has been at the Stanford University School of Medicine Medical Center and Packard Children’s Hospital as chief of pediatric urology. Since 1993, she has also been director of the Urology Residency Program at Stanford, and has been successful in recruiting more women physicians to her specialty. She noted that the numbers have grown rapidly; when she got her board certification in urology in 1983, there were only fifteen women urologists in the U.S. Now there are more than two hundred.
Linda M. Dairiki Shortliffe, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Dr. Paula L. Stillman
While teaching pediatrics at the University of Arizona in the 1970s, Paula Stillman needed a reliable way to evaluate her students’ clinical competence. Her solution was to train and use “patient instructors” or “standardized patients.” Stillman’s system is a competency based program, Objective Structured Clinical Evaluations (OSCE), developed to assess medical students, foreign medical graduates, and U.S. doctors in danger of losing their licenses. Her system has also been adopted by medical schools in China.
Paula L. Stillman, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 3 of 0
Dr. Paula L. Stillman
Dr. Paula L. Stillman developed a tool that is used to evaluate the clinical competence of medical students, foreign medical graduates, and U.S. doctors in danger of losing their licenses.
Click on the video play button to watch an interview with Dr. Stillman.
-
ReadBiography
-
Transcript
I faced my first obstacle the first day of medical school, and I remember sitting with three men in my class around a cadaver, as part of a gross anatomy course. And one of the men said to me, “You took the place of one of my friends, and because you’re here, he didn’t get into medical school. And this is not a place for women. Women should be home and taking care of the house.” So that was an introduction to medical school. And what I decided after that was that I was going to work very hard and become a very good student, and try to amount to something with my career, so that I wouldn’t feel I was taking anybody’s place but I was there rightfully, on my own. Before we developed the standardized patient concept, the evaluation of clinical skills was very subjective. Students were either good or not good. They would occasionally be observed by an attending physician, but there wasn’t a reproducible, reliable, valid way of assessing these skills and documenting whatever weaknesses existed, and then providing corrective feedback and education to the student. This technique allowed students to be compared to an absolute standard, and to have individualized feedback, and multiple observations by experienced people. I was motivated to create this method of teaching and evaluating because I wanted to make sure that there was an opportunity for students and residents to really learn these very critical clinical skills, and not perpetuate mistakes. I wanted somebody who was knowledgeable to be able to provide immediate feedback to them, and tell them what they did well, what they didn’t do well, and make sure that they did it better the next time. When I went to medical school there were very few career paths that were open to women, and most of the women in my class went into pediatrics because it was very acceptable for us to do that. The other acceptable field at that time was psychiatry. Young women today who go into medicine can do anything. They can be surgeons, they can do whatever they want to do, and they have lots of options, which we didn’t have so many years ago.
-
Copy Link
Copied

Close Menu ITEM 4 of 0
Dr. Edithe J. Levit
In 1986, The Association of American Medical Colleges (AAMC) bestowed their Special Recognition Award on Dr. Edithe J. Levit, the first woman president and CEO of a national medical association, the National Board of Medical Examiners. Dr. Levit introduced new technologies and strategies for the examination of medical students, spearheading change to improve standards. Carefully managing the needs of both medical schools and examiners, she promoted dynamic changes that included the introduction of audiovisual tools, computer–based exams, and the first self–assessment test of the American College of Physicians.
Edithe J. Levit, M.D
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 5 of 0
Dr. Edithe J. Levit
Dr. Edithe J. Levit established new ways to evaluate doctors’ clinical competence and was the first woman president of a national medical association, the National Board of Medical Examiners.
Click on the video play button to watch a video on Dr. Levit.
-
ReadBiography
-
Transcript
Dr. Edithe J. Levit became the first woman president and CEO of a national medical association when she took over the leadership of the National Board of Medical Examiners. The Board was founded in 1915 to create national standards for medical licensing and education. Dr. Levit was responsible for making sure that the board kept up with changing times and the most useful innovations that could help measure students’ abilities. She was hired in the 1960s as one of the board’s first full-time medical professionals. Over the decades, she instituted creative innovations that have revolutionized the way medical students are evaluated. Among her many innovations were PMPs... or “Patient Management Problems.” They were designed to test how well medical students make decisions while examining and taking the history of a patient. PMPs became a highly effective way to test all students on the same skills, and hold them to the same standards. Dr. Levit later introduced computer-based testing, audiovisual tools such as films of meetings with patients, and the first self-assessment test of the American College of Physicians. Dr. Levit was successful in ushering in such sweeping changes by consistently proving their efficacy, and eloquently justifying a new approach. Within the first ten years, she rose through the ranks and in 1977, became President and CEO of the National Board of Medical Examiners. In 1986, Dr. Levit received the first ever Honorary Resolution from the American Medical Association’s Resident Physician Section for her commitment to the highest standards in medical education. She also was honored with a Special Recognition Award from the Association of American Medical Colleges. As Dr. Levit recalls, “I spent the last 25 years of my career with the National Board of Medical Examiners... those years were the most stimulating, creative, and rewarding time of my professional life.”
-
Copy Link
Copied

Close Menu ITEM 6 of 0
Dr. Rita Charon
As director of the program in humanities and medicine and the clinical skills assessment program at Columbia University’s College of Physicians and Surgeons, Rita Charon, M.D., developed an innovative new teaching method. The “parallel chart” system brings literature and medicine together to improve the doctor–patient relationship, and forms part of the only narrative competency course in a United States medical school.
Rita Charon, M.D., M.A., Ph.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 7 of 0
Dr. Rita Charon
Dr. Rita Charon pioneered a form of medical education that incorporates literature to help clinicians better understand the patient experience.
Click on the video play button to watch an interview with Dr. Charon.
-
ReadBiography
-
Transcript
Dr. Edithe J. Levit became the first woman president and CEO of a national medical association when she took over the leadership of the National Board of Medical Examiners. The Board was founded in 1915 to create national standards for medical licensing and education. Dr. Levit was responsible for making sure that the board kept up with changing times and the most useful innovations that could help measure students’ abilities. She was hired in the 1960s as one of the board’s first full-time medical professionals. Over the decades, she instituted creative innovations that have revolutionized the way medical students are evaluated. Among her many innovations were PMPs... or “Patient Management Problems.” They were designed to test how well medical students make decisions while examining and taking the history of a patient. PMPs became a highly effective way to test all students on the same skills, and hold them to the same standards. Dr. Levit later introduced computer-based testing, audiovisual tools such as films of meetings with patients, and the first self-assessment test of the American College of Physicians. Dr. Levit was successful in ushering in such sweeping changes by consistently proving their efficacy, and eloquently justifying a new approach. Within the first ten years, she rose through the ranks and in 1977, became President and CEO of the National Board of Medical Examiners. In 1986, Dr. Levit received the first ever Honorary Resolution from the American Medical Association’s Resident Physician Section for her commitment to the highest standards in medical education. She also was honored with a Special Recognition Award from the Association of American Medical Colleges. As Dr. Levit recalls, “I spent the last 25 years of my career with the National Board of Medical Examiners... those years were the most stimulating, creative, and rewarding time of my professional life.”
-
Copy Link
Copied

Close Menu ITEM 8 of 0
Dr. Barbara Bates
Barbara Bates further developed the role of the nurse–practitioner, and wrote a guide to patient history–taking that has become the standard text for health practitioners and medical students. Her book, Guide to Physical Examination and History Taking, first published in 1974, has been published in several revised editions and includes a twelve–part video supplement, A Visual Guide to Physical Examination.
Barbara Bates, 1990
Joan E. Lynaugh, Ph.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 9 of 0
Dr. Barbara Bates
Dr. Barbara Bates wrote Guide to Physical Examination and History Taking, a standard text for health practitioners, and helped to develop the role of the nurse practitioner.
Click on the video play button to watch a video on Dr. Bates.
-
ReadBiography
-
MedlinePlus
-
Transcript
Dr. Barbara Bates changed how medical professionals learn the skills of physical examination and diagnosis. And, she developed the role of Nurse-Practitioners. At the University of Rochester in the 1970’s, she came to think that special training could prepare nurses to share with doctors some of the responsibilities of patient care. She also became particularly interested in how physicians are trained to diagnose patients. As she taught the skills of physical examination and clinical thinking, she realized the standard teaching text used by students was not user-friendly. She began meeting with a group of ten nurses and five physicians. They called themselves “The Clandestine Group,” and they worked to completely re-think the teaching guides. The result of their efforts was a hand-drawn, informative, and easy-to-use text for nurse-practitioner students. The book’s organization was based on the popular bird-watching guide by Roger Tory Peterson. Introductory chapters addressed interview techniques, taking notes on health history, common and important symptoms, and assessment of mental health. Specific chapters also made it easy to look up anatomy and physiology. Techniques for physical exams were described in detail. The first edition of Dr. Bates’s “Guide to Physical Examinations and History Taking” was published in 1974. Since then it has become a standard textbook for nursing and medical training programs.
-
Copy Link
Copied

Close Menu ITEM 10 of 0
Dr. Barbara Ross-Lee
Barbara Ross–Lee, D.O., has worked in private practice, for the U.S. Public Health Service, and on numerous committees, and in 1993 was the first African American woman to be appointed dean of a United States medical school.
Barbara Ross–Lee, M.A., D.O.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 11 of 0
Dr. Barbara Ross-Lee
Dr. Barbara Ross–Lee was the first African America woman to be appointed dean of a U.S. medical school.
Click on the video play button to watch an interview with Dr. Ross–Lee.
-
ReadBiography
-
Transcript
A lot of the obstacles that I faced growing up were based upon things that I can’t change, the fact that I’m a minority and a female. When you grow up as a poor, black female in this society, certainly at that time, you’re never that confident that you will achieve your dreams. You just want to be successful at whatever direction you take. And you tend to run a broken-field course. There’s no straight path to where you want to get to, because the opportunities were never there in kind of a laid-out fashion for you. It was quite an experience to live in the segregated South. You’d go to movie theaters and you had to sit in the balcony, you couldn’t sit downstairs. We could not utilize the library, so I couldn’t read, and I was already an avid reader. But the worst part I think about it was the way in which you were demeaned when you went into public facilities. That you couldn’t drink out of faucets, and you couldn’t go to bathrooms, and the kind of stern, controlled training that my mother and my aunt at the time gave us—to never allow yourself to be so vulnerable that you have to demean yourself to utilize these facilities. And I saw a lot of things happen to people that could have been prevented. And I saw a lot of hopelessness as it related to health care that should not be allowed to exist. And so to a large extent, when I got the opportunity to go back to medical school, it was this population that I wanted to address. The ones that I can make a difference with. I think that experience in the South began to formulate this resolve, this personal resolve that I would never let the external environment define who I was. When I became the dean of Ohio University College of Osteopathic Medicine the media notified me that I was the first African American dean of an American medical school. It caught me off guard. I had no idea. To think that in the late 90s, that we’re still looking at women and at minorities as being “first,” it caused me to pause, and to be somewhat disappointed. But it also immediately then meant that I had to take the position seriously, and really utilize it to keep the doors open for other women, and for other minorities. Because clearly there weren’t enough of us, if I happened to be the first.
-
Copy Link
Copied
Changing Medicine, Changing Life
Confronting the multiplying challenges of health care, women physicians have joined the highest ranks of medical administration and research. As leaders, they make choices that benefit communities across America and around the world. As healers, they identify and respond to many of the most urgent crises in modern medicine, from the needs of underserved communities, to AIDS and natural and man–made disasters.
Their influence reaches across the profession out into our lives, redefining women’s roles and society’s responsibilities. By changing the face of medicine, women physicians are changing our world.
Changing Medicine, Changing Life
Caring for People
Calling upon the art as well as the science of medicine, women physicians treat the whole patient and the whole spectrum of health care needs. The perspectives they bring to care for the living and comfort for the dying encompass all aspects of the medical and emotional well–being of the healthy, the ill, and the at–risk.
This multifaceted approach is reshaping the way that both practitioners and patients strive to improve the quality of life and deal with disease and injury, while widening the scope of medical care for individuals and communities.

Close Menu ITEM 0 of 0
Dr. Lori Arviso Alvord
Dr. Lori Arviso Alvord bridges two worlds of medicine—traditional Navajo healing and conventional Western medicine—to treat the whole patient. She provides culturally competent care to restore balance in her patients’ lives and to speed their recovery.
Lori Arviso Alvord, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
-

Navajo blanket
Navajo blanket designs incorporate many patterns and have become increasingly vibrant as newer, cheaper dyes have been developed. Making a three by five foot rug–shearing the sheep, spinning the wool, dying the yarn, weaving the textile–takes at least three hundred hours to complete. These blankets are sold around the world as valuable works of art.
Lori Arviso Alvord, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
-

Corn pollen pouch
In Navajo tradition, corn pollen is collected by dusting it off the corn tassel for use in prayers and healing. In Dr. Alvord’s description of the ninth and final evening of the Night Chant healing ceremony, a young patient sprinkles corn pollen on groups of dancers.
Lori Arviso Alvord, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
-

Navajo sandpainting
Navajo sandpaintings are used in healing or blessing ceremonies. They can be made with crushed stone, crushed flowers, gypsum, pollen, sand, and dyes. After the experience, the paintings are respectfully destroyed. Permanent sandpaintings are an art form, and do not feature the sacred imagery used in ceremonially.
Lori Arviso Alvord, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
-

Bear pendant
The Organization of Student Representatives, a student branch of the Association of American Medical Colleges, presented this pendant to Dr. Alvord as a gift after she delivered a lecture.
Lori Arviso Alvord, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
-
Learning about Dr. Alvord’s Heritage

Close Menu ITEM 2 of 0
Dr. Elizabeth Kübler-Ross
Elisabeth Kübler–Ross, a Swiss–born American psychiatrist, pioneered the concept of providing psychological counseling to the dying. In her first book, On Death and Dying (published in 1969), she described five stages she believed were experienced by those nearing death—denial, anger, bargaining, depression, and acceptance. She also suggested that death be considered a normal stage of life, and offered strategies for treating patients and their families as they negotiate these stages. The topic of death had been avoided by many physicians and the book quickly became a standard text for professionals who work with terminally ill patients. Hospice care has subsequently been established as an alternative to hospital care for the terminally ill, and there has been more emphasis on counseling for families of dying patients.
Ken Ross Photography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 3 of 0
Dr. Margaret Hamburg
Margaret Hamburg, one of the youngest people ever elected to the Institute of Medicine (IoM, an affiliate of the National Academy of Sciences), is a highly regarded expert in community health and bio–defense, including preparedness for nuclear, biological, and chemical threats. As health commissioner for New York City from 1991 to 1997, she developed innovative programs for controlling the spread of tuberculosis and AIDS.
Margaret Hamburg, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 4 of 0
Dr. Margaret Hamburg
Dr. Margaret Hamburg is a leader in public health who developed programs for controlling the spread of tuberculosis and HIV/AIDS in the 1990s.
Click on the video play button to watch an interview with Dr. Hamburg.
-
ReadBiography
-
MedlinePlus
-
Transcript
I discovered my true passion when I shifted out of the clinical setting and moved into public health. People used to sometimes ask me, “Don’t you feel like you’ve thrown away all that medical training? You’re not taking care of patients anymore.” And instead, I feel like I’ve just expanded my universe of patients, and I’m not just focused one-on-one, but really looking at the needs of whole populations. And when I was New York City’s Health Commissioner, for example, I had almost eight million patients! During the period when I was dealing with HIV/AIDS there was this extraordinary realization of our vulnerability to infectious diseases, and new diseases that we’d never seen before, and also the recognition that diseases like AIDS had many, many aspects that had nothing to do with medicine and medical care. And I really got interested in working at the intersection of medicine and social and legal and economic issues. I really came to understand that you couldn’t effectively address health simply by working within the medical system. When I was in New York City as Health Commissioner, I first got interested and concerned about the threat of biological weapons. I was Health Commissioner actually the first time that the World Trade Center was bombed, so the possibility of domestic terrorism was very real to me. I started thinking about domestic terrorism as it related to the subject closest to my heart— health, medicine, and infectious disease—and I immediately could identify all kinds of vulnerabilities to biological agents intentionally used to do harm. And so we actually began a program in New York City when I was there to prepare against the possible threat of bioterrorism, but we saw it as the extreme end of the spectrum of infectious disease threats that we faced. In the biological program here at NTI (Nuclear Threat Initiative) we are focused on a couple of critical activities. A portion of our efforts and resources are focused on prevention, and nonproliferation of biological weapons, and funding programs and trying to help develop policies to address those concerns. But given how hard it may be, ultimately, to prevent the use of a biological agent as a weapon, we also have to think about how can we recognize it and respond as quickly and as effectively as possible.
-
Copy Link
Copied

Close Menu ITEM 5 of 0
Dr. Leona Baumgartner
From 1954 to 1962, Leona Baumgartner, M.D., served as the first woman commissioner of New York City’s Department of Health. She used her position to bring no–nonsense health and hygiene advice to millions of Americans via regular television and radio broadcasts, and by sending health care professionals to visit schools and church groups. Throughout her career she broadened the scope of public health by teaching preventive medicine in easy–to–understand brochures, and helped to improve the health of New York’s poorest and most vulnerable.
National Library of Medicine, Images from the History of Medicine, B02511
-
ReadBiography
-
DigitalCollections
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 6 of 0
Dr. Leona Baumgartner
Dr. Leona Baumgartner was the first woman to become commissioner of the New York City Department of Health and pioneered health education programs and health services in poor communities.
Click on the video play button to watch a video on Dr. Baumgartner.
-
ReadBiography
-
MedlinePlus
-
Transcript
Throughout her career, Dr. Leona Baumgartner found innovative ways to capture the public’s attention and deliver her message of good health and hygiene. Elvis Presley was even persuaded to pose for a photograph as he received his polio vaccination to encourage young people to participate in the vaccination program. Dr. Baumgartner began her career in public health during the Depression, working as a pediatric intern in New York City. Home visits in Manhattan’s poorest neighborhoods brought her face to face with the effects of poverty. The families she visited often could not get basic medical care or afford healthy foods. In 1937, Dr. Baumgartner joined the New York Department of Health. She was director of public health training, and taught child and school hygiene. She rose through the ranks, coordinating city-wide health services, disease clinics, school health programs, and parenting education classes. She visited professional groups and spoke out at public forums, talking to parents and health care professionals about keeping children healthy. In 1954, Dr. Baumgartner was appointed Health Commissioner of New York City— the first woman ever to hold the job. She appeared regularly on television, teaching about preventive medicine and became the well-known face of public health in New York City. Her public appeals were key to the success of health campaigns for vaccination and fluoridation. Throughout New York, Dr. Baumgartner and her staff inspected food products and restaurants, and posted information about sanitary practices in the workplace. To aid health care workers in communicating with immigrant mothers, her staff trained midwives to be aware of cultural differences. She also worked with President Lyndon B. Johnson to reverse government policy and provide funding for birth control programs in other countries. Dr. Leona Baumgartner has been hailed as “one of those amazing women who managed to juggle several appointments and careers while maintaining a family and social life.” Her lifelong dedication to public health, combined with her tact and diplomacy, made her influential at the highest levels of government.
-
Copy Link
Copied

Close Menu ITEM 7 of 0
Dr. Christine Karen Cassel
“Pursuing difficult questions — in science and in policy — takes one to interesting places,” says Christine Cassel, M.D., a renowned expert in geriatric medicine and medical ethics. She works to improve quality of life for elderly patients, challenging out–of–date ideas about what can be expected in the aging process.
Christine Karen Cassel, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 8 of 0
Dr. Christine Karen Cassel
Dr. Christine Karen Cassel is a leading expert in geriatrics and medical ethics and was the first woman president of the American College of Physicians.
Click on the video play button to watch an interview with Dr. Cassel.
-
ReadBiography
-
MedlinePlus
-
Transcript
When I first began in this field, the standard rounds we would make in the hospital: we would come in, talk with the patient, listen to their heart and their lungs, maybe feel the abdomen. If the patient was in a wet bed it wasn’t our problem, it was a nursing problem. You would leave the room never knowing whether the patient was able to walk or not. And if the patient was confused, all too often you said, “Well, that’s sundowning, that happens with older people.” So the whole range of functional issues that really make a difference between whether an elder person can live alone, or has to be in a nursing home, were things that we didn’t have a clue about how to address. Urinary incontinence, mental confusion, and walking or ambulation, and the strength of somebody’s ability to get themselves to the bathroom, or even out of bed. And maybe I’m just a sensible woman or something, but it just seemed to me there needed to be a lot more attention on these common problems of older people, which we weren’t learning enough about. And so the idea of having a field of geriatric medicine where I could do that, that would be morally needed and make a contribution to people who needed help. At the same time that it would be full of important ethical issues that needed study and analysis, and that were philosophically challenging. The reason why intergenerational connection is so important is to give real meaning and vitality to our aging society. Because we’re moving from a society where a hundred years ago 5 percent of the population was over 65, to 20 years from now 20 percent of the population will be over 65. That means one out of five people, everywhere you go—in the movie theaters, in the grocery stores, in the airports, on the golf courses— wherever you are, are going to be “senior citizens.” To marginalize and make irrelevant one-fifth of the population is just not a smart thing for our society to do. Plus, people are healthier and more independent as they age these days, and that’s going to continue, too. So we can’t afford as a society not to take advantage of the skills and contribution of that whole segment of our population. So it’s very important to me that we find ways that younger people can interact with older people, to counteract stereotypes, ageism, negative attitudes about their own aging, and to help reinforce the connections within their own families. Many of my colleagues in medicine say to me, “How can you do this. It’s so depressing, and it’s so frustrating, because nobody ever gets better.” Well, if you look at most of medicine, there are very few dramatic cures anymore. What we’ve done is we’ve managed to make people able to live better with chronic illness—with heart disease, even with cancer. And geriatrics is just like that. When you help somebody live better, with multiple medical problems, or even help them die better, at the end of their life, their family and that patient are hugely grateful. And I find it very rewarding and so I tell people "what do you mean?" I think this is actually a very rewarding and satisfying field.
-
Copy Link
Copied

Close Menu ITEM 9 of 0
Dr. JoAnn Elisabeth Manson
Dr. JoAnn Manson has been a leading researcher in the two largest women’s health research projects ever launched in the United States—the first large scale study of women begun in 1976 as the Harvard Nurses’ Health Study, and the National Institute of Health’s Women’s Health Initiative, which involved 164,000 healthy women. Until the early 1990s, research on human health was usually done from all–male subject groups, and the results generated were thought to apply to both sexes. Federal regulation now mandates the inclusion of women in all research studies, as men and women may react differently to certain diseases and drug remedies, a fact Dr. Manson’s research efforts have helped to establish.
JoAnn Elisabeth Manson, M.D., Dr.P.H.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 10 of 0
Dr. Joann Elisabeth Manson
Dr. JoAnn Elizabeth Manson is a leading researcher in women’s health and public health.
Click on the video play button to watch an interview with Dr. Manson.
-
MedlinePlus
-
Transcript
When I was in medical school in the late 1970s, it was very common to use the male model for teaching. For instance, there was the classical “70 kilogram man,” and you know, the doses of drugs that would be used for a male of that body size, and also the risk factors for diseases, and the treatment of various diseases in males. The Nurses’ Health Study was started in 1976, with 121 thousand female registered nurses. It was really the first large-scale observational study of women, looking at risk factors for many chronic diseases— breast cancer, colon cancer, heart disease, diabetes, and previously, most of these studies had been in men. I feel very strongly that there needs to be more of an emphasis on prevention and health promotion than there’s been in the past. The paradigm has been treatment of disease, more so than prevention. And there is increasing evidence that lifestyle factors play an enormous role in prevention of disease. I’ve often said that regular physical activity is as close to a magic bullet for good health as we’ve come in modern medicine, despite all the technological advances. The list of conditions that can be prevented or at least improved through regular exercise is really an expansive one. You’re talking about reduced risk of diabetes, heart disease, stroke, obesity, several forms of cancer— particular colon cancer and breast cancer, osteoporosis, and many others. And the portfolio is enormous. Our understanding of the benefits of exercise also has evolved over the years. We used to believe that vigorous and prolonged exercise was necessary in order to improve health. That you needed to get your heart rate at least 70 to 80 percent maximum, you needed to do the exercise continuously, at least 20 minutes, 3 times a week, and it had to be quite vigorous. We now know that even moderate intensity exercise, such as brisk walking— and it can be broken up into maybe 15 minutes or even 10 minutes at a time—can have important health benefits including the prevention of heart disease, and stroke, and diabetes, and various forms of cancer, and osteoporotic fractures. So I think we’re learning more and more about the benefits of moderate exercise—which is good news from a public health standpoint. Because many people will not engage in vigorous exercise. And setting the bar too high, can serve as a deterrent of getting started.
-
Copy Link
Copied

Close Menu ITEM 11 of 0
Dr. JudyAnn Bigby
JudyAnn Bigby, M.D., is director of the Harvard Medical School Center of Excellence in Women’s Health. She is devoted to the health care needs of underserved populations, focusing especially on women’s health. She is also nationally recognized for her pioneering work educating physicians on the provision of care to people with histories of substance abuse.
JudyAnn Bigby, M.D., Photo by Michael T. Quan and Courtesy of Patriots Trail Girl Scout Council
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 12 of 0
Dr. JudyAnn Bigby
Dr. JudyAnn Bigby serves as the director of Harvard Medical School’s Center of Excellence in Women’s Health and works to address the health care needs of vulnerable populations.
Click on the video play button to watch an interview with Dr. Bigby.
-
ReadBiography
-
MedlinePlus
-
Transcript
I see patients part-time. I only spend two mornings a week seeing patients. And with all my other responsibilities, I keep doing that because my patients are the ones who inspire me. I see mostly women. I have a lot of women of color, who may not be that well off, and you know, they are really incredible people. They have a lot of adversity in their lives—they are very ill, many of them, but they have so much positive that they think about their lives. So that’s one thing that keeps me going and inspires me. One of the things that I am trying to do is to try to get physicians to see things from the patient’s perspective. Not just how it feels to have a heart attack, or breast cancer, or something like that. But also how the circumstances of a patient’s life impacts everything that happens to them, from the moment they walk into a health care facility. It may determine how comfortable they feel speaking to the secretary. It may determine how comfortable they feel asking a doctor a question. It may impact how comfortable they feel accepting instructions or advice from a doctor. They may decide that because of a past experience, or a family member’s experience, that they aren’t going to trust that doctor and not follow the advice. In our study, where we were trying to find out what types of things contribute to dissatisfaction with doctors by women of color—Black and Latina women—we found that both doctors and patients make assumptions about each other. The women seemed more aware that they were making the assumptions; they felt that race was a very important issue in the way that they built their assumptions. The doctors did not feel that they were making assumptions based on race, but on other issues. But in the end, what happens is, because of these assumptions, when the two individuals are communicating, they’re not communicating about it the same way. Their assumptions are different. It definitely colors the way they interact with the other person. And I think that one of the things that needs to happen is people need to be able to recognize their assumptions and talk about them, so that people can get on the same page when they’re communicating. For those people who are worried that healthcare is such a negative field now—because of managed care, or not being paid enough money, or having a lot of pressure to see more patients—I think that we need people to go into medicine who will turn around and say, “Well, if this is not the right way to do it, if this is not best for the patients, then we have to change.” And we need more people like that.
-
Copy Link
Copied
Changing Medicine, Changing Life
Transforming the Profession
Many women physicians strive to balance their personal and professional lives, as well as the needs of individual patients and entire communities. They are promoting reforms to eradicate the professional barriers that many of them faced in their own careers and working to change the way that medicine is taught and practiced.
Drawing on their own interests and experiences, women physicians are instituting changes that have far–reaching benefits for the health and happiness of families, communities, and medical practitioners themselves.

Close Menu ITEM 0 of 0
Dr. Perri Klass
As a pediatrician, writer, wife, and mother—Perri Klass has demonstrated how medicine is integral to the health of families and communities, and how doctors themselves struggle to balance the conflicting needs of profession, self, and family. With her love of literature and her involvement with literacy, Klass is acutely aware of the importance of reading to personal and professional success. As medical director of Reach Out and Read, a national program which makes books and advice about reading to young children part of every well–child visit, she encourages other pediatricians to foster pre–reading skills in their young patients.
Reach Out and Read National Center
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Susan M. Briggs
Susan M. Briggs, a trauma surgeon at Massachusetts General Hospital, established and became the first director of the International Medical Surgical Response Team (IMSuRT), an emergency response team that, on short notice, organizes and sends teams of doctors, nurses, and other health professionals from throughout New England to emergencies around the globe.
Susan M. Briggs, M.D., M.P.H.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Dr. Edith Irby Jones
In 1948, nine years before the “Little Rock Nine” integrated Central High School in Little Rock, Arkansas, Edith Irby Jones became the first black student to attend racially mixed classes in the South, and the first black student to attend the University of Arkansas School of Medicine. Her enrollment in a previously segregated southern medical school made news headlines across the nation.
Edith Irby Jones, M.D.
Edith Irby Jones, M.D.
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 3 of 0
Dr. Edith Irby Jones
Dr. Edith Irby Jones was the first woman to be elected president of the National Medical Association and the first African American to graduate from University of Arkansas School of Medicine (now the University of Arkansas for Medical Sciences.)
Click on the video play button to watch an interview with Dr. Jones.
-
MedlinePlus
-
Transcript
I really didn’t think about when I applied to medical school that there was a possibility of my not being accepted. The University of Arkansas was one of the ones that was on my list to apply to. It didn’t dawn on me that there might be a question about my race. It was close to home, but MOST of all why I accepted it— it had a tuition of 500 dollars. On the day of orientation, Dr. Schenalt, the dean at that time called me in and said, “We have some situations. The state law requires us...” At that time, blacks and whites could not eat together in a public situation. They could not use the same toilet facilities, by state law. So I accepted that. I didn’t have any choice. I was not trying to desegregate, I was not trying to change any laws, I felt... I just wanted a medical education. The kitchen help would always put on fresh flowers every day. A change of flowers, never the same. It either came from their yard, or from someplace, but always... never a word spoken, never an encouraging word saying, “we’re proud of you,” nothing said, nothing to say “if you need help, come to us,” none of that. It was just a sort of unspoken, “we are here.” The reason that I have stayed in Houston, and the reason that I have stayed in “third ward” Houston, is because it allows me to do what I want to do. I see those who cannot afford to go to the other areas, even in Houston, to get medical care. I see those who cannot pay a parking fee because there is a charge for parking. I see people who are ashamed to go in and say, “I don’t have any money, but I’m sick.” People give me my passion. To be able to encourage someone who would not have achieved their potential. To be able to help the physical body to heal, that would not have been healed, or a family would have lost that member. To send someone off having the same feeling that I have— that the world is mine.
-
Copy Link
Copied

Close Menu ITEM 4 of 0
Dr. Leah J. Dickstein
Psychiatrist Leah J. Dickstein is a former president of the American Medical Women’s Association and vice president of the American Psychiatric Association. Her innovative Health Awareness Workshop Program, at the University of Louisville, is based on her experience attending medical school while raising a family. The popular program, which covers everything from individual well–being to personal relationships, as well as race and gender issues, has made the University of Louisville one of the nation’s most family–friendly medical colleges.
Leah J. Dickstein, M.D., M.A.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 5 of 0
Dr. Leah J. Dickstein
Dr. Leah J. Dickstein developed a program to help medical students balance their studies and family lives and was president of the American Medical Women’s Association.
Click on the video play button to watch a video on Dr. Dickstein.
-
ReadBiography
-
MedlinePlus
-
Transcript
For six years, Leah Dickstein taught sixth grade in Brooklyn, to help support her family while her husband, Herbert Dickstein, attended medical school. After he had completed his training, Leah Dickstein enrolled in medical school, and the couple came up with a range of strategies to balance the responsibilities of caring for their three children while building their careers. Leah Dickstein had a clear sense of her own priorities, and so Saturdays and summers were saved for family activities, which she considered more important than graduating at the top of her class. Dr. Herbert Dickstein brought the boys to the hospital to visit Dr. Leah Dickstein when she was on call during her residency. Over the years, she developed other ways to cope with the everyday challenges of combining a career in medicine with family life. Those experiences led her to develop an innovative program to teach medical students and their partners how to cope with the demands of medical school—while maintaining their relationships and family commitments. Since 1981 she has been the Director of the Health Awareness Workshop. Her program addresses everything from study skills and time management to community resources, mentoring, exercise, and nutrition. The message is that students must take care of their own physical and mental health before they can learn to take care of others. Dr. Leah Dickstein’s work has made the University of Louisville one of the most family-friendly medical colleges in the nation.
-
Copy Link
Copied

Close Menu ITEM 6 of 0
Dr. Barbara Barlow
Barbara Barlow was the first woman to train in pediatric surgery at Babies Hospital, Columbia University Medical Center (now called Babies’ and Children’s Hospital of New York). By researching and documenting the causes of injuries to children in Harlem, and increasing public education about their prevention, she has helped to dramatically reduce accidents and injuries to inner–city children in New York and throughout the United States.
Barbara Barlow, M.D., M.A.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 7 of 0
Dr. Barbara Barlow
Dr. Barbara Barlow founded the Injury Free Coalition for Kids and helped increase public education on how to prevent childhood injuries.
Click on the video play button to watch an interview with Dr. Barlow.
-
ReadBiography
-
MedlinePlus
-
Transcript
In 1975 I came to Harlem as Chief of Pediatric Surgery. I wanted to work in a public hospital, because I didn’t want to do private practice. I wanted to offer medical care to children who perhaps would not get it because they couldn’t afford to pay, or because they had poor insurance, and so I looked at the public hospitals in New York City, and I chose Harlem. As Director of the Service, of course, I knew every child who came into the hospital and so I saw children falling out windows, being hit by cars, being injured in playgrounds. And in those days, we had a lot of children being shot and assaulted. And I felt that there must be some way we can make this community safer for children because this is not an appropriate thing to happen to anyone’s child. When children came in severely injured, dying from injuries, permanently disabled from injuries—it broke my heart. Really. I used to cry with the parents, and I couldn’t bear anymore to see this happening without trying to do something to make things better. So I constantly wrote grants to find funding to make an Injury Prevention Program that would involve the community and would make it a safer place for children. Basically, what the staff did, is they went block to block and mapped the community. We didn’t find any commercial maps of Harlem in those days. The maps of Manhattan cut off at 110th Street, so that we had to make our own maps. So we knew where the playgrounds were, where the schools were, where the churches were, so we would understand the community block by block, and we did that. And we also used consumer product safety standards, and evaluated every playground in Harlem, and we took pictures. And of course, they all violated consumer product safety standards. And while we did that, we involved the community in the process. We all have a responsibility to people in the community. Everybody has a responsibility for building good communities, good places to raise children. Everybody has a responsibility to see that every child has a chance in this life, has a good education, has good after-school things to do, good sports, good recreation— that’s all our responsibilities. Not just the doctors’. Harlem is a very special community. It’s like a small town. And they said maybe it was so successful because it was Harlem. My career as a pediatric surgeon and as a surgeon has been so enriched by my work in the community, with the community, for children. I would have never been able to predict this when I was a student. But it came naturally, in the course of what I was doing and what I was seeing.
-
Copy Link
Copied

Close Menu ITEM 8 of 0
Dr. Marianne Schuelein
As a pediatric neurologist at Georgetown University Hospital in the 1960s and 1970s, Dr. Marianne Schuelein came to understand the problems of affordable child care from her own experience as a working mother. In 1973, as vice president of the District of Columbia chapter of the American Woman’s Medical Association, she decided to present the issue directly to Albert Ullman (D–Oregon), chair of the Ways and Means Committee of the U.S. House of Representatives. In 1976, Congress passed a law allowing child care tax deductions, enabling more women to work outside the home.
Marianne Schuelein, M.D.
Marianne Schuelein, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 9 of 0
Dr. Marianne Schuelein
Dr. Marianne Schuelein campaigned for childcare tax deductions, which Congress pass into law in 1976, enabling more women to work outside the home.
Click on the video play button to watch an interview with Dr. Schuelein.
-
ReadBiography
-
Transcript
I knew from when I was very young that I wanted to do something useful. I think that was my main goal. I remember once telling a guidance counselor I wanted to find my place in society. And that didn’t mean society with a capital S, it meant I wanted to do something for the society. She misunderstood me. I liked science, I was good at science. When I was quite young, maybe 12, I loved horseback riding, and I memorized all the bones of a horse because I wanted to. But I also was thinking at one time of being a social worker. And the combination of science and social work— the most logical thing seemed to be medicine. In the 60s, when I had my first child, I earned about $15,000 a year. About half of that went for childcare most of the rest went for income tax. I thought this was particularly difficult. I was fortunate to be making at least $15,000, but most of my contemporaries couldn’t make that much, and a lot of them didn’t work for that reason. And I felt that something really needed to be done about it. Somebody suggested that I make an appointment with the head of the House Ways and Means Committee. So I met him and I told him what I thought. We perhaps met together for 10 or 15 minutes, and I went home and nothing happened for a while. But within the next few years childcare did become, at least in part, deductible. Some years ago I was at a party and met a woman who had been his assistant. When we were introduced she said, “I know your name. You were the one who was influential in getting the bill passed that allowed women to deduct childcare.” You don’t have to have connections, you don’t have to money, you don’t have to have a high office. You can make things change. One should never assume that things cannot be changed. When things are wrong, they can always be changed, that’s what people do. And it only takes somebody with enough passion, with enough bulldog perseverance to make that difference.
-
Copy Link
Copied
Changing Medicine, Changing Life
Taking the Lead
In recent decades, women physicians have risen to the very top ranks of the institutions that lead medical research and define the highest standards of practice. Deciding which issues to focus upon, they direct research and funding and are instrumental in implementing the policies, developing the drugs and treatments, and drafting the legislation to meet emerging medical challenges.
From high–profile, influential positions, women physicians provide examples and encouragement, as well as career opportunities, for other women who hope to practice medicine.

Close Menu ITEM 0 of 0
Dr. Antonia Novello
When Dr. Antonia Novello was appointed Surgeon General of the United States by President George Bush in 1990, she was the first woman—and the first Hispanic—ever to hold that office. Her appointment came after nearly two decades of public service at the National Institutes of Health, where she took a role in drafting national legislation regarding organ transplantation.
Antonia Novello M.D., M.P.H., Dr.P.H.
Antonia C. Novello, M.D., M.P.H., Dr.P.H.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 1 of 0
Dr. Catherine D. DeAngelis
In her role as the first woman editor of the Journal of the American Medical Association, Catherine DeAngelis, M.D., has made a special effort to publish substantive scientific articles on women’s health issues. The journal plays an important role in bringing new research to light, and featured articles can lead to fundamental changes in treatment. Under her editorship, the journal published a landmark study questioning the benefits of hormone replacement therapy in 2002. She also served as editor of the Archive of Pediatrics and Adolescent Medicine, from 1993 to 2000.
Catherine DeAngelis
Catherine DeAngelis, M.D., M.P.H.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied

Close Menu ITEM 2 of 0
Dr. Ruth L. Kirschstein
As director of the National Institute of General Medical Sciences from 1974 to 1993, Dr. Ruth Kirschstein was the first woman institute director at the National Institutes of Health (NIH). Throughout her career, she has worked as an administrator, fundraiser, and scientific researcher, investigating possible public health responses in the midst of crisis and conservatism.
Ruth L. Kirschstein, M.D.
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 3 of 0
Dr. Ruth L. Kirschstein
Dr. Ruth L. Kirschstein served as director of the National Institute of General Medical Sciences, becoming the first woman director of an institute at the National Institutes of Health (NIH).
Click on the video play button to watch an interview with Dr. Kirschstein.
-
ReadBiography
-
Transcript
I wanted to be a doctor from a very young age, even before I went to high school. And I’m not sure exactly what motivated me. I had a father who was a chemist. I had a mother who was extremely ill through most of my childhood, and spent a long time in the hospital. It may have been that, that motivated me partly, as well. When I applied for medical school women were not very commonly applying for school—I actually applied to every medical school in the United States. At least one of them wrote me and said, “We only take men.” And that sort of was not a very good thing, and it didn’t make me very happy. Today, over 50 percent of each medical school class are women. When I went to medical school it was a very small number in my class, which started in 1947, which was the first post-World War II class. It actually had 10 out of 110, which was pretty big, but when you think about it, 5 of them were nurses who had been in the military, were able to get the GI Bill to go to medical school, and decided they didn’t really want to answer to anybody else anymore— they wanted to be their own bosses. So it is a real difference now. In addition, Ph.D. biological and chemical scientists make up about 40 percent of our graduate programs in those areas. But the problem is that women are still not in sufficient leadership positions in medical schools and in universities. There are very few women deans of medical schools. There are not many chairwomen of departments, and where we have been very successful, and I am absolutely thrilled, there are something like ten women presidents of major universities—we need more. If you have a population of leaders who are all men, they are never going to think of women. They are never going to think of minorities. They are only going to think of people like themselves. And so that told me, when I got the job as director of the National Institute of General Medical Sciences, that I had to see that we changed the culture. And that we thought about women for jobs, and we thought about minorities for jobs. Actually, people said to me when I became the director of NIGMS—the National Institute of General Medical Sciences—people said, “Well, you’re going to hire only women.” And I said, “No; I’m going to give women an equal opportunity to men. But I don’t believe in having an institute that’s all men or all women. We are equal.” And so I did that, quite deliberately.
-
Copy Link
Copied

Close Menu ITEM 4 of 0
Dr. Helen M. Ranney
Dr. Helen Ranney’s landmark research during the 1950s was some of the earliest proof of a link between genetic factors and sickle cell anemia. She went on to become the first woman to chair the department of medicine at the University of California, San Diego, and was the first woman president of the Association of American Physicians from 1984 to 1985.
Helen M. Ranney, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 5 of 0
Dr. Helen M. Ranney
Dr. Helen M. Ranney made pivotal contributions to sickle cell anemia research and became the first woman president of the Association of American Physicians.
Click on the video play button to watch an interview with Dr. Ranney.
-
ReadBiography
-
MedlinePlus
-
Transcript
During my career in medicine, I practiced probably what would be mostly called academic medicine. I had a research program in addition to a clinical program. In the clinical program I saw patients who had ’hematologic,’ that is, blood, disorders. These would be patients who had diseases of the red blood cells—sickle cell anemia, or thalassemia, some patients who had leukemia or who had bleeding disorders. In my class in medical school there was a class of 120 and there were 5 women. And that was about standard, plus or minus a few— that was about standard for most of the Ivy League schools. I don’t think that one was aware of being treated differently than men by any of the faculty. There were clearly some of the students who rather resented the fact that there were women in the class, but you know, one didn’t really take that terribly seriously. They were the kind of students one didn’t take seriously. I think that probably I was slower to be recognized academically then I would have been, had I been a man... but I didn’t really notice it. I never really cared about whether I was an associate professor or not. The only place where I was sure that I probably was discriminated against was at times in the salary scales. At times it was fairly clear to me that men of the similar rank, and if anything, somewhat lesser accomplishment, were making more money. And I was aware that that happened from time to time. On the other hand, I had enough money, so it didn’t really matter. I was offered the position in San Diego because they wanted a chair of the department of medicine, and it, again, was a new school. My devotion has been to new things that were getting started. There was a lot to be done, and a lot of new faculty to be recruited, and a lot of building to be done. I think it’s important to mentor the young physicians who are interested in research, and who need some time to get the tools, the necessary tools, and to learn how the research is done. And also how grants are obtained, and how grants are administered, and how the American system requires some administrative kind of role model for a person who’s entering it for the first time.
-
Copy Link
Copied

Close Menu ITEM 6 of 0
Dr. Audrey Forbes Manley
Dr. Audrey Forbes Manley received a music scholarship to study at Spelman College in Atlanta. She took the opportunity to expand her education and interests and moved into the sciences. She was appointed Assistant Surgeon General in 1988, and is the first African American woman to hold a position of that rank in the United States Public Health Service. In 1997, she returned to Spelman, after forty years in medicine, to serve as president of the college.
Parklawn Health Library
-
ReadBiography
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 7 of 0
Dr. Audrey Forbes Manley
Dr. Audrey Forbes Manley was the first African American woman to achieve the rank of assistant surgeon general (Rear Admiral in the Public Health Service.)
Click on the video play button to watch an interview with Dr. Manley.
-
ReadBiography
-
Transcript
There were several such instances in my life and my professional career, where I was not only the first African American, but the first African American woman, and a couple of occasions I was the first woman. There’s always, I think, a lot of pressure to perform, to be better than the best, because you realize— at least I always felt—that you are opening a door. You also are setting a record. You are setting a watermark. You are setting an expectation. I was the first African American woman to be appointed as an Assistant Surgeon General in the U.S. Public Health Service. And this is a service that is more than 200 years old. That’s quite significant. Again, opening the door, setting a precedent. That you have to perform, because you are then opening the doors for other people. And if you don’t, you can easily, just as easily, close that door. An M.D. degree really prepares you to do anything in the world that you want to do. It is so very basic. The understanding of the body, the mind, how it functions, growth and development, the stages of life. With me, it was that, plus the experience in the Public Health Service. I think that either one without the other would not have prepared me to be a college president. If you’re only thinking of yourself—what material and monetary things you can get, if the Mercedes and the fur coat and the big house is what’s keeping you going— you’re not going to make it. Not too long. You’ll have some immediate successes. But for the long term, for life, you really have to have goals that are bigger than you, family, that have to deal with society and making a contribution that’s bigger than yourself.
-
Copy Link
Copied

Close Menu ITEM 8 of 0
Dr. Frances K. Conley
In 1966, Frances Krauskopf Conley became the first woman to pursue a surgical internship at Stanford University Hospital, and in 1986, she became the first tenured full professor of neurosurgery at a medical school in the United States. In 1991, she risked her career when she drew public attention to the sexist environment which, she argued, pervaded Stanford University Medical Center.
Frances K. Conley, M.D., M.S.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 9 of 0
Dr. Frances K. Conley
Dr. Frances K. Conley was the first woman to be a full tenured professor of neurosurgery at a medical school in the United States.
Click on the video play button to watch an interview with Dr. Conley.
-
ReadBiography
-
MedlinePlus
-
Transcript
I had a number of professors who tried to talk me out of my decision to pursue a career in surgery, and I’m not exactly sure why, although I think that their perception of the lifestyle of the surgeon was not compatible with being a woman. At that point I was married, and I’m sure that the general assumption at that time was that if you’re married you are going to have a family, and that the two—a career in surgery and having a family—were incompatible. Surgery is just such fun. It is a wonderful discipline because you get a chance to do your thinking beforehand. You have to make fairly rapid decisions, and you have to live by those decisions. And what I really enjoyed about it was the planning and execution of "the perfect case." Of doing things meticulously, correctly, efficiently, and having a very happy outcome with it. And one’s ego gets very involved in surgery. And I guess my ego needed to be fed, and surgery did that for me very well. In 1991, I gave up my position as a tenured full professor of neurosurgery at the Stanford Medical School. And I did so because a person was elevated to be the chair of my department who I felt was a very sexist person. The dean had articulated the desire to create an environment at the medical school that was more hospitable to those of us who were different—i.e., women and minorities. And his putting this person into a position of the deanship was antithetical to what he had espoused as his intent. And so I quit. I had tremendous power at that particular time. I was a tenured full professor. And there were very few tenured full professors that were women who were neurosurgeons. I had been elected to a number of things at the University so I was very well known, and had a lot of support behind me, so that I dealt my hand with a fair amount of power behind it. The difference that I made when I took a stand on looking at or exploring the differential treatment that women received in medicine—the difference was, that it woke people up. All of a sudden, that which had been just accepted as part of the medical world, as normative behavior—that you can pat nurses on their butts, and you call people "honey" in front of patients, and that you can do this—that was normative behavior, and nobody questioned it. And I think the difference that I created was it made people stop in their tracks, and it made them think, Hey, is this right? Am I treating my women patients the same way I do my men patients—with respect, and with dignity—and am I giving them as much of me as I should be giving them? And so from that point of view, yes, I think it did make a big difference. Did I correct things? No, not totally.
-
Copy Link
Copied

Close Menu ITEM 10 of 0
Dr. Bernadine Healy
Cardiologist Bernadine Healy is a physician, educator, and health administrator who was the first woman to head the National Institutes of Health (NIH). Known for her outspoken, innovative policymaking, Dr. Healy has been particularly effective in addressing medical policy and research pertaining to women.
Bernadine Healy, M.D.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 11 of 0
Dr. Bernadine Healy
Dr. Bernadine Healy was the first woman to direct the National Institutes of Health (NIH).
Click on the video play button to watch an interview with Dr. Healy.
-
ReadBiography
-
MedlinePlus
-
Transcript
My parents, and particularly my father, thought it was wonderful for a woman to be a doctor. And in those days, when I was growing up, it was really exceptional, unusual, for a woman to pursue a career in medicine. And as far as my father was concerned, it was the perfect place for me to go. It was a place where I could use my intelligence and my hard work, but also make a difference. When I went to Harvard Medical School there were roughly 10 percent— less than 10 percent—of the class were women. And in those days—although they probably don’t like to remember this— medical schools had quotas, and there was the prevailing attitude that women were taking up a spot that wasn’t necessarily going to be used as well as a spot filled by a man. Women had to have, I think, better academic credentials, and often go through much tougher screening. When I was at NIH (National Institutes of Health), there were a number of wonderful challenges, and a number of very difficult ones... the Women’s Health Initiative, which I, believe it or not, announced to the Congress of the United States roughly three weeks after I was Director, in which I said, “We need a moon walk for women.” And I laid out the general concept of the Women’s Health Initiative. That it would be holistic. That it would involve not one organ, or one disease, but in fact, major illnesses and issues of wellness that affect women—particularly in that over-50 range where most women, most people, face their illnesses, and see their lives demolished, often, by diseases that often can be prevented. Something that really paid attention to that huge gap in our knowledge, our clinical and our basic knowledge. I saw 9/11 through very, very personal, up-close experiences. And one of the things that I came away from that experience with is the incredible role that we, as physicians—because of our knowledge and our experiences, one-on-one with human beings, at the most critical time in their lives—how physicians can bring a certain comfort, just by being physicians, to people at that time. Not always to patients, but to people. I think any young person who is thinking about a career in medicine, should keep thinking. It is one of the most extraordinary careers, and one of the most amazing intellectual journeys—because medicine is something that keeps you humble all the time, because there’s always new information that makes you challenge yesterday’s thinking. It is something that is also so humane. I mean all of us, I believe, in our hearts are humanitarian. And how wonderful to be in a career that in almost any dimension of it—whether you’re the doctor at the bedside, or the scientist in the laboratory, or the public health doc tracking down the latest epidemic—that you are doing something that is pure in it’s fundamental purpose, which is helping another human being. And you may not always see that.
-
Copy Link
Copied

Close Menu ITEM 12 of 0
Dr. Paula A. Johnson
Dr. Paula Johnson is a women’s health specialist and a pioneer in the treatment and prevention of cardiovascular disease. She conceived of and developed one of the first facilities in the country to focus on heart disease in women.
Brigham and Women’s Hospital
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 13 of 0
Dr. Paula A. Johnson
Dr. Paula A. Johnson is a pioneering specialist in cardiovascular disease and developed one of the first facilities dedicated to heart disease in women.
Click on the video play button to watch an interview with Dr. Johnson.
-
ReadBiography
-
MedlinePlus
-
Transcript
About a year ago, I become the executive director for the (Mary Horrigan) Connors Center for Women’s Health and Gender Biology, and it was really a dream come true. The mission of the center is to improve the health of women, and to transform medicine, so that sex and gender are routinely applied, where appropriate, in medicine. And it’s a pretty lofty goal... a pretty lofty mission, but it is absolutely inspiring to me. We are working in the clinical venues here at the Brigham and Women’s, not just in traditional women’s health areas, but really in every area of medicine that touches women. Whether it be all the surgical areas, whether it be medical subspecialties, and of course obstetrics and gynecology, to really think about what is it that women need? What are the models of care that we need to implement, not just in women’s health practices, but throughout our institution, and can that then serve as a model? Especially if we can measure it for other institutions to improve the health of women. We do a lot of work in partnership with our community women, where we really know that the rates of heart disease are far higher than they should be. Black women, for example, in our neighborhood—the neighborhood of Brigham and Women’s—die at a rate of four times that of their Caucasian counterparts, at a very young age. And this is kind of in the middle of what some people would call the “medical Mecca.” So we do a lot of work with our community women, to think about risk factor reduction. But to also think about what do they need in order to stay healthy? What do they need in order to understand and cook differently? And that might include, quite frankly, better incomes. And therefore how do we connect with other groups around what is kind of the basic standard by which we should be thinking women should live, in order to maintain and achieve health? When you are starting from behind, and medicine is moving forward at a lightning pace—how do you catch up, but then continue to move forward, so that you’re not continuously behind? And I think that we’re always talking about closing the gap. But closing the gap becomes much more difficult year after year. Because we’re not closing it, and medicine is moving forward. And I think there is just an inherent challenge there that we have not figured out. And I think it becomes even more difficult when you begin to talk about a stressed economic environment, and one in which the greater public may not recognize, (or appreciate or understand) the full degree of barriers that are out there for African Americans to achieve that health state.
-
Copy Link
Copied

Close Menu ITEM 14 of 0
Dr. Joan Y. Reede
Dr. Joan Reede works to recruit and prepare minority students for jobs in the biomedical professions, and to promote better health care policies for the benefit of minority populations. In 2001, she became Harvard Medical School’s first dean for diversity and community partnership. She is the first African American woman to hold that rank at HMS and one of the few African American women to hold a deanship at a medical school in the United States.
Joan Y. Reede, M.D., M.P.H., M.S.
-
ReadBiography
-
MedlinePlus
-
EnlargeImage
-
Copy Link
Copied
Close Menu ITEM 15 of 0
Dr. Joan Y. Reede
Dr. Joan Y. Reede was appointed Harvard Medical School’s first dean for diversity and community partnership and has worked to bring more minority students into the health professions.
Click on the video play button to watch an interview with Dr. Reede.
-
ReadBiography
-
MedlinePlus
-
Transcript
I’m dean for Diversity and Community Partnership at Harvard Medical School. And it is designed to bring more diversity to the faculty at Harvard Medical School and its affiliated teaching hospitals—and there are 17 affiliated institutions— and to look at diversity efforts at the student, the resident, the faculty, and staff levels. But it also looks at engaging the community, and how we can work better with our surrounding community. But the truth of the matter is, if you’re going to bring diversity into medicine, you can’t just look at the faculty that are there—people at the end of the pipeline, because the numbers are too small. And so what you have to do is put in place programs that will bring more students into science. Help them understand the joy of science. Help them understand that you can love science, and do anything! So what we’ve put together at Harvard is a series of programs that says you have to address the total pipeline. And at the same time put together programs that say that it is part of our responsibility to our surrounding community. I think for youth today it can be very hard. And it can be very daunting to think “I have to match the achievements of someone else.” And so I think the first thing is to figure out, what is it that you like doing? What is it that you want to do? What do you want your life to be about? And then to understand that it’s going to take a lot of hard work. You can accomplish anything. I see people of color moving into positions that my mother, my grandmother, never dreamed would happen. I see young women who are doing amazing things, and leading amazing things. And that’s only going to grow. It’s not going to lessen over time, it’s going to grow. So I think there are more and more opportunities out there, and no one should let anyone, at any point in time, tell them what they can’t do.
-
Copy Link
Copied
-
Dr. Maude Elizabeth Seymour Abbott
-
Dr. Jill Nina Afrin
-
Dr. Tenley E. Albright
-
Dr. Hattie Elizabeth Alexander
-
Dr. Virginia M. Alexander
-
Dr. Ethel D. Allen
-
Dr. Lori Arviso Alvord
-
Dr. Dorothy Hansine Andersen
-
Dr. Kathryn Dorothy Duncan Anderson
-
Dr. Jean R. Anderson
-
Dr. Marcia Angell
-
Dr. Kathleen R. Annette
-
Dr. Virginia Apgar
-
Dr. Vivia Belle Appleton
-
Dr. Linda Susan Aranaydo
-
Dr. Carol A. Aschenbrener
-
Dr. Linda S. Austin
-
Dr. Mary Ellen Avery
-
Dr. Emily Partridge Bacon
-
Dr. S. Josephine Baker
-
Dr. Barbara Barlow
-
Dr. Emily Dunning Barringer
-
Dr. Doris Gorka Bartuska
-
Dr. Barbara Bates
-
Dr. Patricia E. Bath
-
Dr. Constance Elizabeth Urciolo Battle
-
Dr. Leona Baumgartner
-
Dr. Lillian M. Beard
-
Dr. G. Valerie Beckles-Neblett
-
Dr. Regina Marcia Benjamin
-
Dr. (Mary) Alice Bennett
-
Dr. Michelle Anne Bholat
-
Dr. Grete Lehner Bibring
-
Dr. JudyAnn Bigby
-
Dr. Elizabeth Blackwell
-
Dr. Emily Blackwell
-
Dr. Karin J. Blakemore
-
Dr. Ruth Harriet Bleier
-
Dr. Susan J. Blumenthal
-
Dr. Jo Ivey Boufford
-
Dr. Nina Starr Braunwald
-
Dr. Clara Arena Brawner
-
Dr. Susan M. Briggs
-
Dr. Benjy Frances Brooks
-
Dr. Anna Elizabeth Broomall
-
Dr. Rowine Hayes Brown
-
Dr. Dorothy Lavinia Brown
-
Dr. U. Diane Buckingham
-
Dr. Judith Martin Cadore
-
Dr. Mary Steichen Calderone
-
Dr. Helen Mary Caldicott
-
Dr. Clair Mills Callan
-
Dr. Selma Harrison Calmes
-
Dr. Alexa Irene Canady
-
Dr. Myrtelle May Canavan
-
Dr. Lucy M. Candib
-
Dr. Consuelo E. M. Carmona
-
Dr. Mary E. Schmidt Case
-
Dr. Christine Karen Cassel
-
Dr. Rita Charon
-
Dr. Alice Drew Chenoweth
-
Dr. Eliza Lo Chin
-
Dr. May Edward Chinn
-
Dr. Donna M. Christian-Christensen
-
Dr. Patricia StandTal Clarke
-
Dr. Emeline Horton Cleveland
-
Dr. Raquel Eidelnan Cohen
-
Dr. Elizabeth D. A. Magnus Cohen
-
Dr. Rebecca J. Cole
-
Dr. Lorraine Hanlon Comanor
-
Dr. Frances K. Conley
-
Dr. Gerty Theresa Radnitz Cori
-
Dr. Rhonda Cornum
-
Dr. Nereida Correa
-
Dr. Molly Joel Coye
-
Dr. Margaret D. Craighill
-
Dr. Rebecca Lee Crumpler
-
Dr. Leigh Ann Curl
-
Dr. Sadye Beatryce Curry
-
Dr. Ruth E. Dayhoff
-
Dr. Catherine D. DeAngelis
-
Dr. Leila Alice Daughtry Denmark
-
Dr. Carolyn R. Denning
-
Dr. Jane F. Desforges
-
Dr. Katherine M. Detre
-
Dr. Helen Octavia Dickens
-
Dr. Nancy Wilson Dickey
-
Dr. Helen Aird Dickie
-
Dr. Leah J. Dickstein
-
Dr. Marie Amos Dobyns
-
Dr. Sarah Reed Adamson Dolley
-
Dr. Joanne Froio Domson
-
Dr. Janice Green Douglas
-
Dr. Ethel Collins Dunham
-
Dr. Harriet Pearson Dustan
-
Dr. Georgia Rooks Dwelle
-
Dr. Sara K. Dye
-
Dr. Ruth Marguerite Easterling
-
Dr. Lena Frances Edwards
-
Dr. Louise Eisenhardt
-
Dr. M. Joycelyn Elders
-
Dr. Martha May Eliot
-
Dr. Lois Taylor Ellison
-
Dr. Mary Jane England
-
Dr. Roselyn Epps
-
Dr. Marie Diana Equi
-
Dr. Angela M. Erdrich
-
Dr. Alice Ettinger
-
Dr. Matilda Arabella Evans
-
Dr. Audrey Elizabeth Evans
-
Dr. Denise L. Faustman
-
Dr. Dorothy Celeste Boulding Ferebee
-
Dr. M. Irené Ferrer
-
Dr. Marcella Farinelli Fierro
-
Dr. Frances McLemore Fisk
-
Dr. Faith Thayer Fitzgerald
-
Dr. Katherine A. Flores
-
Dr. Judith Flores
-
Dr. Virginia Davis Floyd
-
Dr. Kathleen M. Foley
-
Dr. Justina Laurena Carter Ford
-
Dr. Jean L. Fourcroy
-
Dr. Virginia Kneeland Frantz
-
Dr. Bernadette T. Freeland-Hyde
-
Dr. Vanessa Northington Gamble
-
Dr. Nancy E. Gary
-
Dr. Marilyn Hughes Gaston
-
Dr. Helene D. Gayle
-
Dr. Beatrice Elizabeth Gee
-
Dr. Julia Louise Gerberding
-
Dr. Jennifer A. Giroux
-
Dr. Nunzia Bettinsoli Giuse
-
Dr. Helen Hofsommer Glaser
-
Dr. Lynn R. Goldman
-
Dr. Eliza Ann Grier
-
Dr. Mary Elizabeth Guinan
-
Dr. Connie Myers Guion
-
Dr. Margaret Hamburg
-
Dr. Alice Hamilton
-
Dr. Margaret Irving Handy
-
Dr. Harriet L. Hardy
-
Dr. Réjane M. Harvey
-
Dr. Florence Pat Haseltine
-
Dr. Elizabeth Dexter Hay
-
Dr. Maxine Hayes
-
Dr. Margaret Caroline Heagarty
-
Dr. Bernadine Healy
-
Dr. Karen Hein
-
Dr. Patricia Nez Henderson
-
Dr. Jane Ellen Henney
-
Dr. Maria Isabel Herran
-
Dr. Jane E. Hodgson
-
Dr. Jimmie C. Holland
-
Dr. Bertha Van Hoosen
-
Dr. Mary Ann Hopkins
-
Dr. Minnie Frances Hayden Howard
-
Dr. Susan Emma Hertz Howard
-
Dr. Mary Catherine Raugust Howell
-
Dr. Christie Ann Huddleston
-
Dr. Gertrude Teixeira Hunter
-
Dr. Kate Campbell Hurd-Mead
-
Dr. Lisa I. Iezzoni
-
Dr. Mary Corinna Putnam Jacobi
-
Dr. Georgiana M. Jagiello
-
Dr. Grace Marilynn James
-
Dr. Lissy Feingold Jarvik
-
Dr. Nancy E. Jasso
-
Dr. Mae C. Jemison
-
Dr. Renee Rosalind Jenkins
-
Dr. Ann Connor Jobe
-
Dr. Carol J. Johns
-
Dr. Paula A. Johnson
-
Dr. Halle Tanner Dillon Johnson
-
Dr. Olga Jonasson
-
Dr. Harriet B. Jones
-
Dr. Mary Amanda Dixon Jones
-
Dr. Edith Irby Jones
-
Dr. Julia M. Jones
-
Dr. Georgeanna Seegar Jones
-
Dr. Elizabeth Karlin
-
Dr. Susan Veronica Karol
-
Dr. Judith Salmon Kaur
-
Dr. Frances Kathleen Oldham Kelsey
-
Dr. Mary Margaret Kemeny
-
Dr. Catharine Gail Kincaid
-
Dr. Mary Elizabeth Dickason King
-
Dr. Ruth L. Kirschstein
-
Dr. Perri Klass
-
Dr. Irena Grasberg Koprowska
-
Dr. Lila Stein Kroser
-
Dr. Elisabeth Kübler-Ross
-
Dr. Elise Depew Strang L'Esperance
-
Dr. Yvette Laclaustra
-
Dr. Joyce Cohen Lashof
-
Dr. Roz D. Lasker
-
Dr. Agnes D. Lattimer
-
Dr. Risa J. Lavizzo-Mourey
-
Dr. Margaret Morgan Lawrence
-
Dr. Elizabeth Theresa Lee-Rey
-
Dr. Marianne J. Legato
-
Dr. Dolores Maria Leon
-
Dr. Edithe J. Levit
-
Dr. Edith M. Lincoln
-
Dr. Iris F. Litt
-
Dr. Hannah E. Myers Longshore
-
Dr. Susan M. Love
-
Dr. Esther Clayson Pohl Lovejoy
-
Dr. Theresa Loya
-
Dr. Amneris E. Luque
-
Dr. D. Joanne Harley Lynn
-
Dr. Catharine Macfarlane
-
Dr. Sharon M. Malotte
-
Dr. Audrey Forbes Manley
-
Dr. JoAnn Elisabeth Manson
-
Dr. Shirley F. Marks
-
Dr. Clara Marshall
-
Dr. Loy McAfee
-
Dr. Melvina L. McCabe
-
Dr. Anita Newcomb McGee
-
Dr. Anne Biship McKusick
-
Dr. Laurie A. McLemore
-
Dr. Barbara J. McNeil
-
Dr. Martha Alicia Medrano
-
Dr. Dorothy Reed Mendenhall
-
Dr. Flavia Elaine Mercado
-
Dr. Maria J. Merino
-
Dr. Doris Honig Merritt
-
Dr. Jean Baker Miller
-
Dr. Lillie Rosa Minoka-Hill
-
Dr. Janet L. Mitchell
-
Dr. Kelly R. Moore
-
Dr. Alma Dea Morani
-
Dr. Kathryn Ann Morsea
-
Dr. Rosalie Slaughter Morton
-
Dr. Carol Cooperman Nadelson
-
Dr. Lillian Heath Nelson
-
Dr. Maria Iandolo New
-
Dr. Kate Pellham Newcomb
-
Dr. Mary Modelle Newman
-
Dr. Carol M. Newton
-
Dr. Jennifer R. Niebyl
-
Dr. Antonia Novello
-
Dr. Elizabeth Odilile Ofili
-
Dr. June E. Osborn
-
Dr. Janet Rose Osuch
-
Dr. Frances Owl-Smith
-
Dr. Judith Ann Pachciarz
-
Dr. Adriana R. Padilla
-
Dr. Conchita Marie Paz
-
Dr. Louise Pearce
-
Dr. Pamela M. Peeke
-
Dr. Fernande Marie Pelletier
-
Dr. Lucille C. Norville Perez
-
Dr. Muriel Petioni
-
Dr. Susan La Flesche Picotte
-
Dr. Vivian W. Pinn
-
Dr. Mary Lake Polan
-
Dr. Deborah Elizabeth Powell
-
Dr. Ann Preston
-
Dr. Deborah Prothrow-Stith
-
Dr. Helen Cordelia Putnam
-
Dr. Fannie Almara Quain
-
Dr. Sylvia M. Ramos
-
Dr. Teresa Ramos
-
Dr. Helen M. Ranney
-
Dr. Joan Y. Reede
-
Dr. Clarice D. Reid
-
Dr. Lynne McArthur Reid
-
Dr. Rachel Naomi Remen
-
Dr. Ina Park Rhee
-
Dr. Karen Schulder Rheuban
-
Dr. Laurel Wysong Rice
-
Dr. Barbara L. Riley
-
Dr. Elena V. Rios
-
Dr. Carolyn Bauer Robinowitz
-
Dr. Merlyn Meneze Rodrigues
-
Dr. Helen Rodriguez-Trias
-
Dr. Irene Elizabeth. Roeckel
-
Dr. Mary Hasbah Roessel
-
Dr. Cecilia M. Romero
-
Dr. Marian Wilkins Ropes
-
Dr. Linda Rosenstock
-
Dr. Barbara Ross-Lee
-
Dr. Yvette Roubideaux
-
Dr. Marilyn A. Roubidoux
-
Dr. Janet Davison Rowley
-
Dr. Florence Rena Sabin
-
Dr. Gloria Elizabeth Sarto
-
Dr. Louise Schnaufer
-
Dr. Edyth Hull Schoenrich
-
Dr. Marianne Schuelein
-
Dr. Rosalyn P. Scott
-
Dr. Jessie Boyd Scriver
-
Dr. Ida Sophia Scudder
-
Dr. Eleanor Gossard Shore
-
Dr. Linda Dairiki Shortliffe
-
Dr. Omega C. Logan Silva
-
Dr. Charlotte Silverman
-
Dr. Marjorie Spurrier Sirridge
-
Dr. Anneliese Lotte Sitarz
-
Dr. Eve Elizabeth Slater
-
Dr. Susan Potts Sloan
-
Dr. Diane Gail Snustad
-
Dr. Nancy L. Snyderman
-
Dr. Jeannette E. South-Paul
-
Dr. Anna Lenore Skow Southam
-
Dr. Edith E. Sproul
-
Dr. Jeanne Spurlock
-
Dr. Lucy Frank Squire
-
Dr. Sarah M. Stelzner
-
Dr. Esther M. Sternberg
-
Dr. Victoria M. Stevens
-
Dr. Paula L. Stillman
-
Dr. Katherine Boucot Sturgis
-
Dr. Judith Lea Swain
-
Dr. Natalia M. Tanner
-
Dr. Helen Brooke Taussig
-
Dr. Caroline Bedell Thomas
-
Dr. Debi Thomas
-
Dr. Lois Pendleton Todd
-
Dr. Adela S. Valdez
-
Dr. Ileana Vargas-Rodriguez
-
Dr. Yvonnecris Smith Veal
-
Dr. Mary Edwards Walker
-
Dr. Sara Ellen Walker
-
Dr. Lila Amdurska Wallis
-
Dr. Rebekah May Wang-Cheng
-
Dr. Ethel Schwartz Weinberg
-
Dr. Virginia Verral Weldon
-
Dr. Nanette Kass Wenger
-
Dr. Laura Ann Williams
-
Dr. Anna Wessels Williams
-
Dr. Marjorie Price Wilson
-
Dr. Mary Ellen Beck Wohl
-
Dr. Norma Spielman Wohl
-
Dr. Stephanie Joan Woolhandler
-
Dr. Jane Cooke Wright
-
Dr. Terri L. Young
-
Dr. Marie E. Zakrzewska

Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Egestas purus viverra accumsan in nisl. Vulputate dignissim suspendisse in est ante in nibh mauris cursus. Consectetur purus ut faucibus pulvinar elementum integer enim neque volutpat. Massa sapien faucibus et molestie ac feugiat sed lectus vestibulum. Id diam vel quam elementum pulvinar etiam. Tristique sollicitudin nibh sit amet commodo nulla facilisi. Odio euismod lacinia at quis risus sed vulputate odio.
-
DigitalCollections
-
Transcript
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.
-
EnlargeImage
-
MedlinePlus
-
Copy Link